Fibromyalgia is widely known for causing chronic pain, fatigue, and cognitive dysfunction. However, many individuals with fibromyalgia also report experiencing frequent infections, such as sinus infections, respiratory illnesses, urinary tract infections, and skin infections.
While fibromyalgia itself is not classified as an autoimmune disease, it appears to have a profound impact on the immune system, potentially increasing susceptibility to recurrent infections.
This article explores the relationship between fibromyalgia and recurrent infections, including possible causes, common infections, and effective management strategies.
1. Why Do People with Fibromyalgia Experience Recurrent Infections?
Recurrent infections in fibromyalgia patients may be due to multiple factors, including:
1. Immune System Dysregulation
✔ Fibromyalgia has been linked to immune system imbalances, where the body struggles to fight off infections effectively.
✔ Some studies suggest low natural killer (NK) cell activity, which weakens the body’s ability to eliminate harmful pathogens.
2. Chronic Stress and Cortisol Imbalance
✔ Long-term stress suppresses the immune system, making individuals more vulnerable to infections.
✔ Many fibromyalgia patients have abnormal cortisol levels, which can impair immune function and increase inflammation.
3. Autonomic Nervous System Dysfunction (Dysautonomia)
✔ The autonomic nervous system (ANS), which regulates involuntary body functions, is often dysregulated in fibromyalgia.
✔ This can affect circulation, mucus production, and inflammatory responses, increasing infection risk.
4. Poor Sleep Quality and Weakened Immunity
✔ Sleep is crucial for a strong immune system, but fibromyalgia patients often suffer from insomnia, restless sleep, or sleep apnea.
✔ Lack of restorative sleep lowers immunity, making the body more prone to infections.
5. Increased Inflammation and Gut Dysbiosis
✔ Fibromyalgia is associated with chronic low-grade inflammation, which may contribute to immune dysfunction.
✔ Many fibromyalgia patients also experience gut issues (like irritable bowel syndrome and leaky gut), which can disrupt gut bacteria balance and weaken immunity.
6. Medication Side Effects
✔ Many fibromyalgia patients take pain relievers, antidepressants, and sleep medications, which may have immune-suppressing side effects.
✔ Some drugs, like corticosteroids, can increase the risk of infections by weakening immune defenses.
2. Common Recurrent Infections in Fibromyalgia
People with fibromyalgia may experience various types of infections more frequently, including:
1. Sinus Infections (Sinusitis)
✔ Chronic congestion and postnasal drip can lead to bacterial sinus infections.
✔ Symptoms include facial pressure, headache, nasal congestion, and yellow or green mucus.
2. Respiratory Infections (Colds, Bronchitis, Pneumonia)
✔ Frequent exposure to viruses can lead to lingering coughs, sore throats, and chest infections.
✔ Many fibromyalgia patients report feeling run down for weeks after a simple cold.
3. Urinary Tract Infections (UTIs)
✔ Fibromyalgia patients, especially women, often experience frequent bladder infections.
✔ Symptoms include burning urination, urgency, and pelvic pain.
4. Yeast Infections (Candida Overgrowth)
✔ Some fibromyalgia patients experience chronic yeast infections, oral thrush, or digestive candida overgrowth.
✔ Symptoms include vaginal itching, white-coated tongue, bloating, and fatigue.
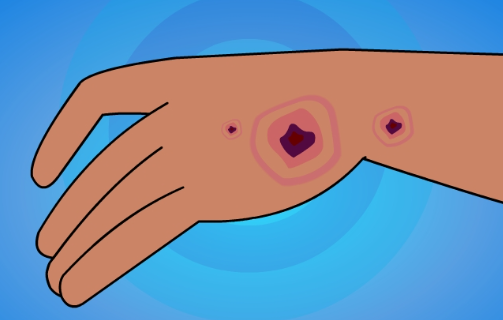
5. Skin Infections (Slow Healing Wounds, Rashes, and Fungal Infections)
✔ Poor circulation and immune dysfunction may cause delayed healing of cuts and frequent skin infections.
✔ Fungal infections like athlete’s foot and ringworm may also be more common.
3. How to Reduce the Risk of Recurrent Infections in Fibromyalgia
While fibromyalgia can make infections more frequent, there are several ways to support immune function and reduce infection risk.
1. Strengthen the Immune System Naturally
✔ Eat a nutrient-dense diet rich in fruits, vegetables, and lean proteins to support immunity.
✔ Include immune-boosting foods like garlic, ginger, turmeric, and fermented foods (probiotics).
2. Improve Sleep Quality
✔ Aim for 7–9 hours of restful sleep per night to allow the immune system to recover.
✔ Consider melatonin, magnesium, or herbal teas to improve sleep.
3. Manage Stress and Reduce Cortisol Imbalance
✔ Practice deep breathing, meditation, or gentle yoga to lower stress levels.
✔ Engage in low-impact exercise like walking or tai chi to support immune function.
4. Support Gut Health
✔ Take probiotics to maintain a healthy gut microbiome and prevent infections.
✔ Avoid excessive sugar, processed foods, and alcohol, which can weaken immunity.
5. Stay Hydrated and Use Humidifiers
✔ Drink plenty of water to keep mucous membranes healthy and reduce sinus infections.
✔ Use a humidifier to maintain moisture levels in dry environments.
6. Reduce Exposure to Infection Triggers
✔ Wash hands frequently and avoid crowded places during flu season.
✔ If prone to sinus infections, use nasal saline rinses to clear mucus buildup.
7. Identify and Address Medication Side Effects
✔ If certain medications are weakening your immune system, talk to your doctor about alternatives.
✔ Avoid unnecessary long-term antibiotic use, which can lead to antibiotic resistance and gut imbalances.
4. When to See a Doctor
If you experience frequent or severe infections, it’s important to seek medical advice. A doctor may:
✔ Run blood tests to check for immune deficiencies or chronic infections.
✔ Test for underlying conditions like autoimmune diseases or chronic viral infections.
✔ Recommend immune-boosting supplements like vitamin C, vitamin D, and zinc.
5. Conclusion: Strengthening Immunity in Fibromyalgia
Recurrent infections are a frustrating and often overlooked aspect of fibromyalgia. While the exact connection remains unclear, immune system dysfunction, poor sleep, stress, and gut imbalances may play a role.
By strengthening the immune system through diet, stress management, better sleep, and lifestyle changes, fibromyalgia patients can reduce their risk of infections and improve overall health.
If infections become chronic or severe, it’s essential to consult a healthcare provider for further evaluation and treatment.
Would you like additional personalized strategies to support your immune system while managing fibromyalgia?

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores