Fibromyalgia is a complex condition that primarily manifests as widespread pain, fatigue, and cognitive dysfunction. However, individuals with fibromyalgia often report a range of other symptoms that affect their overall quality of life, including digestive issues. These digestive disorders can be a challenging aspect of the condition, yet they are not always discussed or linked to fibromyalgia. In this article, we will explore how digestive disorders present in fibromyalgia, the symptoms associated with them, the potential causes, and strategies for managing gastrointestinal discomfort.
What is Fibromyalgia?
Fibromyalgia is a chronic disorder that involves widespread musculoskeletal pain, along with fatigue, sleep disturbances, and cognitive difficulties often referred to as “fibro fog.” It is believed to be related to an abnormal response in the central nervous system, causing heightened pain sensitivity and a range of physical and emotional symptoms. While the hallmark symptoms of fibromyalgia are physical in nature, many individuals also experience other complications, including gastrointestinal (GI) issues, which can contribute to additional discomfort and frustration.
Understanding the Gastrointestinal Impact of Fibromyalgia
Digestive disorders are not uncommon among individuals with fibromyalgia, with many patients reporting symptoms such as bloating, constipation, diarrhea, and abdominal pain. These digestive issues can vary in severity and are often misunderstood as being unrelated to fibromyalgia. However, research suggests that fibromyalgia and gastrointestinal disturbances may be linked due to overlapping factors, including autonomic nervous system dysfunction, inflammation, and stress.
Fibromyalgia and gastrointestinal problems share several common features, such as chronicity, variability in symptom presentation, and the potential to worsen with stress. These overlapping characteristics suggest that the digestive issues experienced by individuals with fibromyalgia are not merely coincidental but may be an intrinsic part of the condition.
Common Digestive Disorders Symptoms in Fibromyalgia
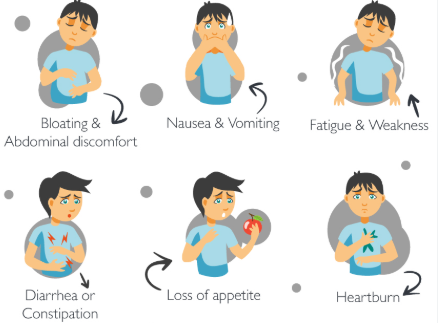
While digestive disorders in fibromyalgia can vary from person to person, the following are some of the most commonly reported symptoms:
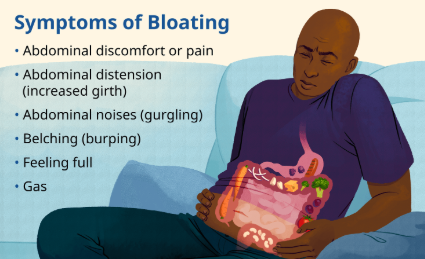
1. Bloating and Gas
Bloating, or the sensation of fullness and distension in the abdomen, is a common digestive complaint among individuals with fibromyalgia. This discomfort is often accompanied by excessive gas, which can lead to a feeling of heaviness or swelling in the stomach area. Bloating may occur after meals, or it may be a more constant issue throughout the day. The feeling of bloating can also contribute to a decrease in appetite and discomfort during routine activities.
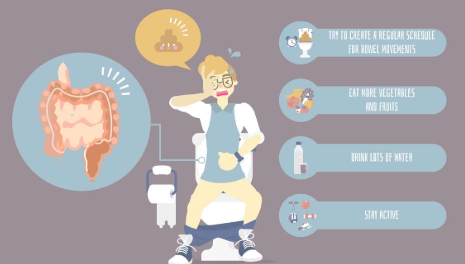
2. Constipation
Constipation is one of the most frequently reported digestive symptoms in fibromyalgia. Individuals with fibromyalgia may experience infrequent bowel movements, hard stools, and difficulty passing stool, leading to discomfort and bloating. Constipation can be particularly bothersome when combined with other symptoms of fibromyalgia, such as fatigue and pain. Individuals may feel as though their digestion is sluggish, and they may experience a sense of fullness or heaviness due to the inability to fully evacuate the bowels.
3. Diarrhea
On the other end of the spectrum, some individuals with fibromyalgia experience diarrhea as a part of their digestive issues. Frequent, loose stools can be unpredictable and distressing, leading to feelings of urgency and a lack of control. Diarrhea can be triggered by stress, certain foods, or fluctuations in the gut’s functioning. For some, the occurrence of diarrhea may alternate with periods of constipation, creating an ongoing cycle of digestive disruption.
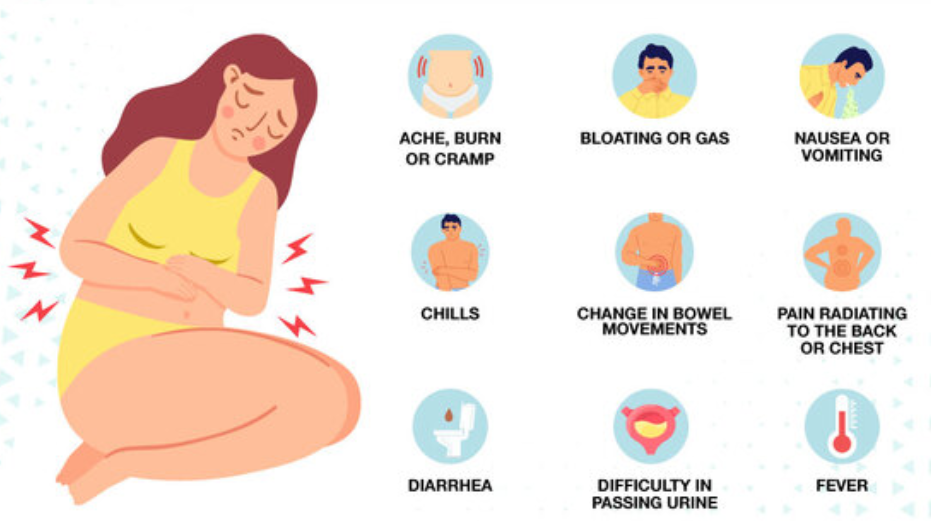
4. Irritable Bowel Syndrome (IBS)-like Symptoms
Irritable Bowel Syndrome (IBS) is a common condition that affects the digestive system, causing symptoms like cramping, bloating, diarrhea, and constipation. Many individuals with fibromyalgia report symptoms similar to IBS, such as abdominal pain, discomfort, and changes in bowel habits. The link between fibromyalgia and IBS is not fully understood, but it is believed that both conditions may share common mechanisms, such as dysfunction in the gut-brain axis and heightened sensitivity to pain signals.
5. Abdominal Pain and Cramping
Abdominal pain and cramping are frequent complaints among individuals with fibromyalgia who experience digestive issues. This pain may range from mild discomfort to severe cramping and may occur after eating or during periods of heightened stress. The pain may be localized to specific areas of the abdomen, or it may feel more generalized. For individuals with fibromyalgia, this abdominal discomfort can be particularly challenging, as it often exacerbates other symptoms such as fatigue and pain.
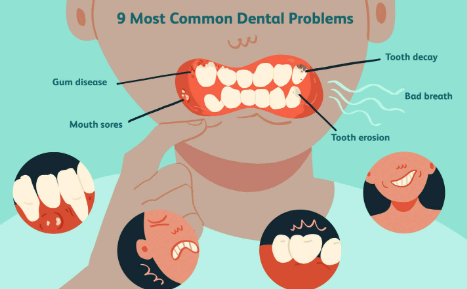
6. Heartburn and Acid Reflux
Some individuals with fibromyalgia may also experience heartburn or acid reflux, which occurs when stomach acid flows back into the esophagus, causing a burning sensation in the chest. This symptom is commonly associated with gastroesophageal reflux disease (GERD). The connection between GERD and fibromyalgia may be linked to factors such as muscle tension, stress, and dysfunction in the autonomic nervous system, all of which are common in individuals with fibromyalgia.
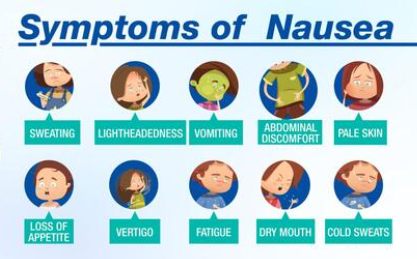
7. Nausea
Nausea, or the sensation of needing to vomit, is another digestive symptom that can be present in fibromyalgia. This symptom may be triggered by food, stress, or other factors, and it can contribute to a reduced appetite and difficulty maintaining adequate nutrition. Nausea may also worsen other fibromyalgia symptoms, such as fatigue, pain, and cognitive dysfunction.
Potential Causes of Digestive Disorders in Fibromyalgia
The exact cause of digestive disorders in fibromyalgia is not fully understood, but several factors may contribute to the development of gastrointestinal symptoms:
1. Autonomic Nervous System Dysfunction
The autonomic nervous system (ANS) plays a crucial role in regulating the digestive system, controlling processes such as motility, enzyme secretion, and blood flow to the gut. In fibromyalgia, there is often dysfunction in the ANS, leading to altered digestive function. This dysfunction may cause irregularities in bowel movements, bloating, and discomfort. Dysautonomia, or the malfunctioning of the autonomic nervous system, is common in fibromyalgia and may contribute to gastrointestinal disturbances.
2. Increased Sensitivity to Pain
Individuals with fibromyalgia are known to have heightened pain sensitivity, a condition called central sensitization. This increased sensitivity can affect the digestive system, making individuals more aware of abdominal discomfort and bloating. The sensation of pain may also be amplified in the gut, leading to more frequent and severe symptoms such as cramping and bloating.
3. Stress and Anxiety
Stress is a well-known trigger for digestive issues, and it can have a profound impact on individuals with fibromyalgia. The chronic pain, fatigue, and unpredictability of fibromyalgia can cause significant emotional and psychological stress, which in turn can exacerbate gastrointestinal symptoms. Anxiety and stress can alter gut motility, increase inflammation, and trigger symptoms such as nausea, diarrhea, or constipation.
4. Gut-Brain Axis Dysfunction
The gut-brain axis refers to the bidirectional communication between the gastrointestinal system and the brain. Research suggests that this communication may be disrupted in individuals with fibromyalgia, leading to gastrointestinal dysfunction. This disruption may contribute to symptoms such as bloating, abdominal pain, and changes in bowel habits. The connection between the gut and the brain is thought to be influenced by factors such as stress, inflammation, and central sensitization.
5. Inflammation
While fibromyalgia is not traditionally considered an inflammatory condition, there is evidence to suggest that low-grade inflammation may play a role in both fibromyalgia and gastrointestinal symptoms. Chronic inflammation can affect the digestive system, contributing to symptoms such as bloating, abdominal pain, and changes in bowel function. Inflammation may also worsen the sensitivity of the gut to normal digestive processes.
Managing Digestive Disorders in Fibromyalgia
While digestive symptoms in fibromyalgia can be distressing, there are several strategies that can help manage gastrointestinal discomfort:
1. Dietary Modifications
Diet plays a significant role in managing digestive issues. Some individuals with fibromyalgia find relief by adopting an anti-inflammatory diet, which includes foods that reduce inflammation and promote gut health. This may include avoiding trigger foods such as dairy, gluten, or processed foods. A fiber-rich diet can also help alleviate constipation, while probiotics may improve gut health and reduce symptoms of bloating and gas.
2. Stress Management Techniques
Since stress is a major contributor to digestive issues, incorporating stress management techniques such as mindfulness, meditation, and deep breathing exercises can be beneficial. These techniques help regulate the autonomic nervous system, reduce inflammation, and promote overall well-being.
3. Exercise
Gentle exercise, such as walking, swimming, or yoga, can help promote healthy digestion and reduce stress. Regular physical activity can improve gut motility, reduce bloating, and alleviate constipation. Exercise also helps improve overall energy levels, which can help manage the fatigue associated with fibromyalgia.
4. Medications
In some cases, medications may be prescribed to manage digestive symptoms. Laxatives, antispasmodics, or medications to reduce acid reflux may be used to address specific gastrointestinal issues. It is important to work closely with a healthcare provider to find the most appropriate treatment plan for managing digestive disorders in fibromyalgia.
Conclusion
Digestive disorders are a common but often overlooked symptom of fibromyalgia. The connection between fibromyalgia and gastrointestinal issues may stem from a variety of factors, including autonomic dysfunction, increased pain sensitivity, stress, and inflammation. By understanding the potential causes of digestive issues and implementing strategies such as dietary modifications, stress management, and gentle exercise, individuals with fibromyalgia can improve their gastrointestinal health and overall quality of life.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores