Fibromyalgia and depression are two complex conditions that often coexist, leading to confusion regarding their differences and similarities. Both can cause chronic pain, fatigue, and cognitive difficulties, but they stem from different underlying mechanisms. Understanding how these conditions differ and how they interact is crucial for accurate diagnosis and effective treatment.
What is Fibromyalgia?
Fibromyalgia (FM) is a chronic pain disorder that affects the way the brain processes pain signals. It is not a psychological disorder, although it can be influenced by mental health factors such as stress and anxiety. Fibromyalgia is considered a central nervous system dysfunction, meaning it amplifies pain perception and often leads to widespread bodily pain.
Common Symptoms of Fibromyalgia:
- Widespread musculoskeletal pain
- Chronic fatigue
- Cognitive issues (often called “fibro fog“)
- Increased sensitivity to pain, noise, light, and temperature
- Sleep disturbances
- Anxiety and depression (as secondary symptoms)
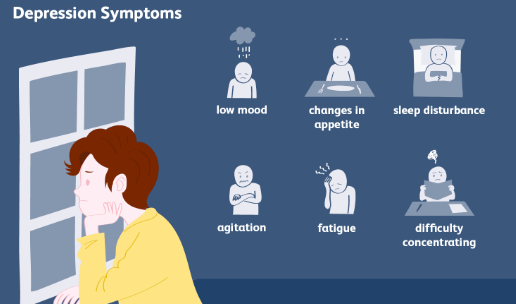
What is Depression?
Depression is a mood disorder that affects emotions, thoughts, and physical well-being. It is characterized by persistent feelings of sadness, hopelessness, and loss of interest in daily activities. While depression can cause physical symptoms such as fatigue and body aches, it originates from chemical imbalances in the brain rather than the nervous system’s pain processing.
Common Symptoms of Depression:
- Persistent sadness or low mood
- Loss of interest or pleasure in activities
- Sleep disturbances (insomnia or excessive sleeping)
- Fatigue or lack of energy
- Difficulty concentrating or making decisions
- Feelings of worthlessness or guilt
- Changes in appetite and weight
- Suicidal thoughts (in severe cases)
Key Differences Between Fibromyalgia and Depression
| Feature | Fibromyalgia (FM) | Depression |
|---|---|---|
| Primary Cause | Central nervous system dysfunction affecting pain processing | Chemical imbalance affecting mood regulation |
| Main Symptoms | Widespread pain, fatigue, cognitive issues | Low mood, loss of interest, changes in appetite and energy levels |
| Pain Presence | Chronic widespread pain | Body aches may occur but are not the primary symptom |
| Fatigue Type | Physical exhaustion, worsened by activity | Mental and physical fatigue, often due to lack of motivation |
| Cognitive Issues | Memory problems, trouble concentrating (fibro fog) | Difficulty focusing due to low mood or apathy |
| Response to Exercise | May worsen pain initially but can help over time | Often improves mood and energy levels |
| Treatment Approaches | Pain management, exercise, sleep improvement, stress reduction | Therapy, antidepressants, lifestyle changes |
The Connection Between Fibromyalgia and Depression
Studies show that 30% to 50% of people with fibromyalgia also have depression. There are several reasons for this overlap:
- Chronic Pain Can Lead to Depression: Living with constant pain can contribute to feelings of helplessness and sadness.
- Neurotransmitter Imbalances: Both conditions are linked to low levels of serotonin, dopamine, and norepinephrine, which regulate pain and mood.
- Sleep Disruptions: Poor sleep quality, common in fibromyalgia, can increase depression risk.
- Shared Risk Factors: Stress, trauma, and genetic predisposition can increase the likelihood of developing both conditions.
Diagnosis Challenges
Because depression and fibromyalgia share some symptoms, such as fatigue, sleep problems, and difficulty concentrating, misdiagnosis can occur. Fibromyalgia is diagnosed based on widespread pain lasting at least three months and the presence of tender points, while depression is diagnosed based on emotional and behavioral symptoms.
Treatment Approaches
Managing Fibromyalgia:
- Medications: Pain relievers, muscle relaxants, and nerve pain medications (e.g., pregabalin, duloxetine)
- Lifestyle Adjustments: Regular exercise, stretching, and maintaining a consistent sleep schedule
- Alternative Therapies: Acupuncture, massage therapy, and cognitive-behavioral therapy (CBT)
Managing Depression:
- Medications: Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs)
- Therapy: Cognitive-behavioral therapy (CBT), psychotherapy, and mindfulness-based interventions
- Lifestyle Changes: Exercise, social engagement, and maintaining a balanced diet
Conclusion
While fibromyalgia and depression share some overlapping symptoms, they are distinct conditions with different causes and treatments. Fibromyalgia is primarily a pain disorder, while depression is a mood disorder. However, their frequent coexistence means that treatment should address both physical and emotional well-being. If you experience symptoms of either condition, seeking medical guidance is essential for an accurate diagnosis and appropriate treatment.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores