Introduction
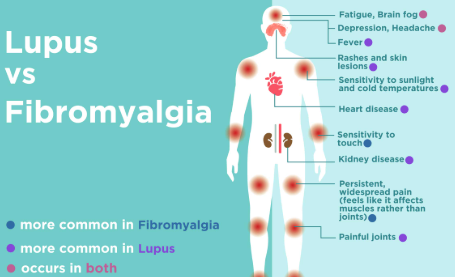
Fibromyalgia is a chronic condition that affects the musculoskeletal system, nervous system, and overall sensory processing. While it is primarily associated with widespread pain, fatigue, and cognitive issues, many individuals with fibromyalgia also experience vision problems. One such concern is glaucoma, a serious eye condition that can lead to permanent vision loss if left untreated.
Glaucoma is caused by increased intraocular pressure (IOP), which damages the optic nerve. This progressive condition can lead to blind spots, tunnel vision, and eventual blindness. Although fibromyalgia itself does not directly cause glaucoma, several factors, such as chronic inflammation, medication side effects, and nervous system dysregulation, may increase the risk of developing this condition.
This article explores the connection between glaucoma and fibromyalgia, the key symptoms to watch for, and the importance of early detection and management.
1. What Is Glaucoma?
Glaucoma is a group of eye diseases that damage the optic nerve, the structure responsible for transmitting visual information from the eye to the brain. The most common cause of glaucoma is elevated intraocular pressure (IOP), which leads to progressive vision loss.
Types of Glaucoma
- Open-Angle Glaucoma – The most common type, characterized by gradual optic nerve damage and slow loss of peripheral vision.
- Angle-Closure Glaucoma – A less common but more severe type that occurs when the drainage system of the eye is blocked, leading to sudden and extreme pressure buildup.
- Normal-Tension Glaucoma – A type where optic nerve damage occurs despite normal eye pressure levels, suggesting vascular or neurological factors may contribute to its development.
Without proper treatment, glaucoma can cause irreversible blindness. However, early detection and treatment can slow its progression and protect vision.
2. How Is Glaucoma Linked to Fibromyalgia?
Fibromyalgia does not directly cause glaucoma, but several underlying factors associated with fibromyalgia may contribute to an increased risk of developing the condition.
2.1 Chronic Inflammation
Inflammation plays a significant role in fibromyalgia and may also contribute to optic nerve damage. Studies suggest that chronic systemic inflammation can impair blood flow to the eyes, making the optic nerve more susceptible to damage.
2.2 Nervous System Dysfunction
Fibromyalgia is associated with autonomic nervous system dysfunction, which can lead to vascular irregularities in the eyes. Blood flow issues may increase the risk of glaucoma by depriving the optic nerve of essential oxygen and nutrients.
2.3 Medication Side Effects
Many individuals with fibromyalgia take medications such as corticosteroids, antidepressants, and anticonvulsants to manage pain, mood disorders, and sleep disturbances. Long-term use of corticosteroids has been linked to increased intraocular pressure, which is a major risk factor for glaucoma.
2.4 Increased Sensitivity to Pressure and Sensory Changes
People with fibromyalgia often experience hypersensitivity to pain and pressure, which may cause them to notice subtle vision changes earlier than others. However, since glaucoma progresses gradually, symptoms may go unnoticed until significant damage has occurred.
3. Symptoms of Glaucoma in Fibromyalgia
The symptoms of glaucoma vary depending on the type and severity of the disease. Fibromyalgia patients, who already experience sensory hypersensitivity and cognitive dysfunction, may find that glaucoma symptoms further impact their daily life and mental well-being.
3.1 Early Symptoms of Open-Angle Glaucoma
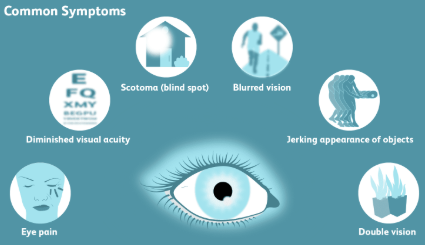
- Gradual loss of peripheral vision (side vision)
- Difficulty seeing objects in low light or dim conditions
- Mild eye strain or discomfort
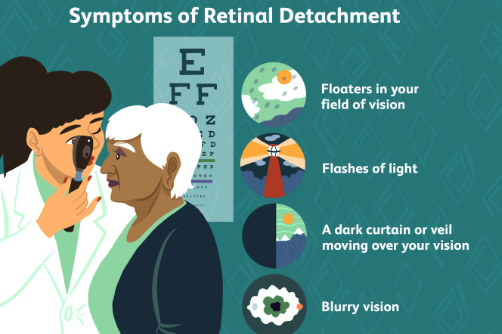
- Blurred vision that comes and goes
3.2 Advanced Symptoms of Open-Angle Glaucoma
- Severe tunnel vision, where central vision remains intact but peripheral vision is nearly lost
- Difficulty adjusting to different lighting conditions
- Blind spots that progressively enlarge
- Increased difficulty with depth perception and balance
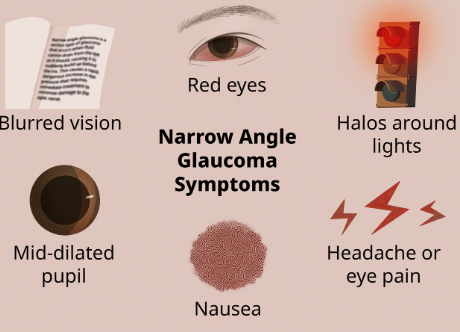
3.3 Symptoms of Angle-Closure Glaucoma (Medical Emergency)
- Sudden, severe eye pain
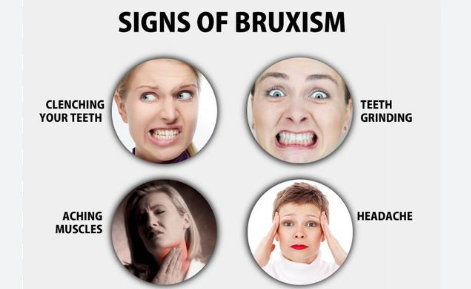
- Headaches and nausea
- Blurry vision or halos around lights
- Redness in the eye
- Rapid vision loss
Angle-closure glaucoma is a medical emergency that requires immediate treatment to prevent permanent blindness.
3.4 Symptoms of Normal-Tension Glaucoma
- Unexplained vision loss despite normal eye pressure
- Frequent eye fatigue or strain
- Difficulty with contrast sensitivity (distinguishing between similar colors or shades)
- Increased light sensitivity
Since fibromyalgia patients often experience vision-related symptoms such as eye strain, blurry vision, and light sensitivity, it is important to differentiate these issues from potential glaucoma symptoms.
4. How Glaucoma Affects Fibromyalgia Patients
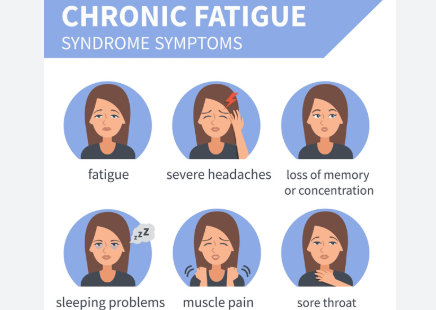
4.1 Increased Visual Fatigue
Fibromyalgia already contributes to eye fatigue, headaches, and cognitive dysfunction. The addition of glaucoma-related vision issues can make everyday activities, such as reading and driving, more exhausting.
4.2 Worsening Light Sensitivity
Many fibromyalgia patients experience photophobia (light sensitivity). Glaucoma can further increase discomfort in bright light, making outdoor activities or working with screens more challenging.
4.3 Impact on Cognitive Function
Fibromyalgia is associated with brain fog and memory difficulties. Vision impairments caused by glaucoma can exacerbate cognitive issues, making it harder to focus and process information.
4.4 Increased Fall Risk
Glaucoma reduces peripheral vision and depth perception, which can lead to poor balance and a higher risk of falls. Since fibromyalgia patients often experience muscle weakness and coordination issues, this can pose a serious safety concern.
5. Diagnosing and Treating Glaucoma in Fibromyalgia Patients
5.1 Diagnosis of Glaucoma
- Comprehensive Eye Exam – Evaluates vision and eye health
- Tonometry Test – Measures intraocular pressure
- Optical Coherence Tomography (OCT) – Scans the optic nerve for damage
- Visual Field Test – Assesses peripheral vision loss
5.2 Treatment Options
- Prescription Eye Drops – Help reduce eye pressure
- Laser Therapy – Improves fluid drainage in the eye
- Surgery – Creates a new drainage pathway for fluid buildup
5.3 Lifestyle Adjustments
- Regular eye check-ups to monitor vision changes
- Eating a diet rich in antioxidants and omega-3 fatty acids to support eye health
- Reducing screen time and taking frequent breaks to ease eye strain
- Wearing blue-light-blocking glasses for computer use
- Engaging in gentle exercise to improve blood circulation
6. Conclusion: Protecting Eye Health in Fibromyalgia
Glaucoma is a serious eye condition that can lead to permanent vision loss if left untreated. While fibromyalgia does not directly cause glaucoma, factors such as chronic inflammation, medication side effects, and autonomic nervous system dysfunction may increase the risk.
Regular eye exams, early detection, and proper treatment are essential to preserving vision. By managing both fibromyalgia symptoms and eye health, individuals can maintain a better quality of life and reduce the risk of severe vision impairment.
Would you like recommendations for natural supplements or alternative therapies to support eye health in fibromyalgia?

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores