Introduction
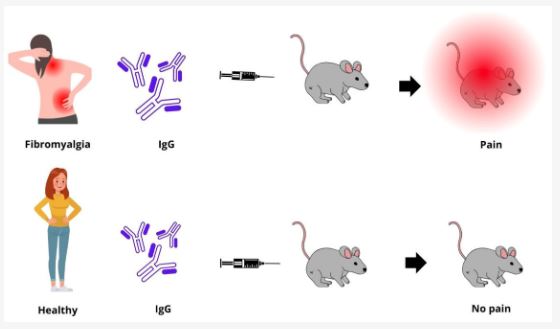
Fibromyalgia syndrome (FMS) is a chronic condition characterized by widespread pain, fatigue, and a range of other debilitating symptoms. Understanding the underlying mechanisms of pain in fibromyalgia is crucial for developing effective treatments. Two key phenomena contributing to the pain experience in fibromyalgia patients are abnormal sensitization and temporal summation of second pain, also known as “wind-up.” This blog post explores these concepts, their role in fibromyalgia, and potential strategies for managing symptoms.
Understanding Fibromyalgia Syndrome
What is Fibromyalgia Syndrome?
Fibromyalgia syndrome is a chronic disorder that affects the musculoskeletal system, leading to widespread pain and tenderness. The exact cause of fibromyalgia is not fully understood, but it involves a combination of genetic, environmental, and psychological factors.
Click Here to Visit the Store and find Much More….
Common Symptoms
- Widespread Pain: Persistent pain affecting multiple areas of the body.
- Fatigue: Chronic tiredness that does not improve with rest.
- Sleep Disturbances: Difficulty falling asleep, staying asleep, or achieving restorative sleep.
- Cognitive Issues: Problems with memory, attention, and concentration, often referred to as “fibro fog.”
- Other Symptoms: Headaches, irritable bowel syndrome, and mood disorders such as anxiety and depression.
Abnormal Sensitization in Fibromyalgia
What is Abnormal Sensitization?
Abnormal sensitization refers to an increased sensitivity to pain stimuli due to changes in the central nervous system. This phenomenon is also known as central sensitization and involves the amplification of pain signals in the brain and spinal cord.
Mechanisms of Abnormal Sensitization
In fibromyalgia, central sensitization results from increased excitability of neurons in the central nervous system, leading to heightened pain perception. This increased excitability can be caused by:
- Neurotransmitter Imbalances: Abnormal levels of neurotransmitters such as glutamate and substance P, which play a role in pain transmission.
- Altered Pain Processing: Changes in the way pain signals are processed and interpreted in the brain and spinal cord.
- Reduced Pain Inhibition: Impaired functioning of the body’s natural pain inhibition mechanisms, leading to an inability to dampen pain signals.
Click Here to Visit the Store and find Much More….
Impact on Fibromyalgia Patients
Abnormal sensitization contributes to the widespread pain experienced by fibromyalgia patients. Even non-painful stimuli, such as light touch or mild pressure, can be perceived as painful due to this heightened sensitivity. This can significantly impact daily activities and quality of life.
Temporal Summation of Second Pain (Wind-Up)
What is Temporal Summation of Second Pain?
Temporal summation of second pain, also known as “wind-up,” is a phenomenon where repeated stimulation of pain receptors leads to an increasingly intense pain response. This occurs due to the cumulative effect of continuous pain signals, resulting in a heightened and prolonged pain experience.
Mechanisms of Temporal Summation
Wind-up occurs when repetitive, low-frequency pain stimuli activate NMDA (N-methyl-D-aspartate) receptors in the spinal cord. This activation leads to:
- Increased Neuronal Excitability: Enhanced responsiveness of spinal cord neurons to pain stimuli.
- Sustained Pain Response: Prolonged activation of pain pathways, leading to a sustained and amplified pain response.
- Pain Memory: The central nervous system “remembers” the pain, making subsequent stimuli more likely to elicit a stronger pain response.
Impact on Fibromyalgia Patients
Temporal summation contributes to the chronic pain experienced by fibromyalgia patients. It can lead to prolonged pain responses to stimuli that would not typically cause long-lasting pain. This phenomenon can exacerbate the overall pain experience and make it more difficult to manage.
Interplay Between Abnormal Sensitization and Temporal Summation
Mutual Reinforcement
Abnormal sensitization and temporal summation can mutually reinforce each other, creating a vicious cycle of chronic pain. The heightened sensitivity from central sensitization makes patients more susceptible to wind-up, while the prolonged pain responses from wind-up further enhance central sensitization.
Clinical Implications
Understanding the interplay between these phenomena is crucial for developing effective treatments. Targeting both central sensitization and temporal summation can help break the cycle of chronic pain and improve symptom management for fibromyalgia patients.
Click Here to Visit the Store and find Much More….
Strategies for Managing Symptoms
Pharmacological Treatments
NMDA Receptor Antagonists
Medications that block NMDA receptors, such as ketamine and memantine, can help reduce temporal summation and alleviate pain. These drugs work by preventing the activation of NMDA receptors, thereby reducing neuronal excitability and wind-up.
Antidepressants and Anti-seizure Drugs
Antidepressants (e.g., amitriptyline, duloxetine) and anti-seizure drugs (e.g., pregabalin, gabapentin) can help modulate pain signals and reduce central sensitization. These medications work by altering neurotransmitter levels and stabilizing nerve activity.
Non-Pharmacological Treatments
Cognitive Behavioral Therapy (CBT)
CBT can help patients manage pain by changing negative thought patterns and behaviors. It can also reduce the emotional impact of pain, helping to break the cycle of central sensitization and temporal summation.
Exercise Therapy
Regular physical activity, such as low-impact aerobic exercises, strength training, and flexibility exercises, can help reduce pain and improve overall function. Exercise promotes the release of endorphins, which are natural pain relievers, and can improve mood and energy levels.
Mind-Body Techniques
Mind-body techniques, such as mindfulness meditation, progressive muscle relaxation, and biofeedback, can help reduce stress and alleviate pain. These practices can improve emotional well-being and enhance the body’s natural pain inhibition mechanisms.
Click Here to Visit the Store and find Much More….
FAQs
What is abnormal sensitization in fibromyalgia?
Abnormal sensitization, or central sensitization, is an increased sensitivity to pain stimuli due to changes in the central nervous system. It involves the amplification of pain signals in the brain and spinal cord, leading to heightened pain perception.
What is temporal summation of second pain (wind-up)?
Temporal summation of second pain, or wind-up, is a phenomenon where repeated stimulation of pain receptors leads to an increasingly intense pain response. This occurs due to the cumulative effect of continuous pain signals, resulting in prolonged and amplified pain.
How do abnormal sensitization and temporal summation impact fibromyalgia patients?
Both phenomena contribute to the chronic pain experienced by fibromyalgia patients. Abnormal sensitization leads to heightened sensitivity, while temporal summation results in prolonged pain responses. Together, they create a cycle of chronic pain that can be difficult to manage.
What pharmacological treatments can help manage these phenomena in fibromyalgia?
NMDA receptor antagonists, antidepressants, and anti-seizure drugs can help reduce central sensitization and temporal summation. These medications work by modulating pain signals and reducing neuronal excitability.
What non-pharmacological treatments are effective for managing fibromyalgia symptoms?
Effective non-pharmacological treatments include cognitive behavioral therapy (CBT), exercise therapy, and mind-body techniques such as mindfulness meditation and progressive muscle relaxation. These approaches can help reduce pain and improve overall well-being.
How can understanding these pain mechanisms improve fibromyalgia treatment?
Understanding the mechanisms of central sensitization and temporal summation can help healthcare providers develop more targeted and effective treatments for fibromyalgia. By addressing both phenomena, it is possible to break the cycle of chronic pain and improve patient outcomes.
Conclusion
Abnormal sensitization and temporal summation of second pain are key phenomena contributing to the chronic pain experienced by fibromyalgia patients. By understanding these mechanisms and their interplay, healthcare providers can develop more effective strategies for managing symptoms. Combining pharmacological treatments with non-pharmacological approaches, such as cognitive behavioral therapy, exercise therapy, and mind-body techniques, can help break the cycle of chronic pain and improve the quality of life for those living with fibromyalgia. Ongoing research and innovation are essential to further enhance our understanding and treatment of this complex condition.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores