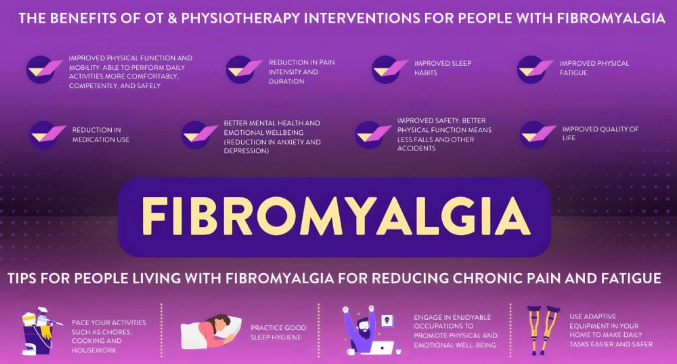
Fibromyalgia is a chronic condition characterized by widespread pain, fatigue, sleep disturbances, and cognitive challenges. While physical symptoms dominate its profile, fibromyalgia also has a profound emotional and psychological impact. Anxiety is a frequent companion to fibromyalgia, often exacerbating symptoms and complicating treatment strategies. Antianxiety agents have emerged as a potential option to address this aspect of fibromyalgia. In this article, we will explore the role of antianxiety agents in managing fibromyalgia, their benefits, limitations, and how they compare to other treatment options.
The Connection Between Fibromyalgia and Anxiety
1. The Prevalence of Anxiety in Fibromyalgia
Research indicates that anxiety disorders are significantly more common in people with fibromyalgia than in the general population. Chronic pain, unpredictable flare-ups, and a reduced quality of life contribute to heightened stress and anxiety.
2. How Anxiety Affects Fibromyalgia Symptoms
Anxiety can amplify the perception of pain and worsen fatigue. It disrupts sleep cycles, leading to poor rest and increased sensitivity to pain. Over time, this creates a vicious cycle where anxiety and fibromyalgia symptoms feed into each other, making effective treatment crucial.
What Are Antianxiety Agents?
Antianxiety agents, also known as anxiolytics, are medications designed to reduce feelings of anxiety, tension, and stress. These drugs work by targeting specific neurotransmitters in the brain to promote relaxation and calmness.
Common Types of Antianxiety Agents
- Benzodiazepines: These fast-acting drugs, such as diazepam (Valium) and lorazepam (Ativan), increase the effect of GABA (a calming neurotransmitter).
- Selective Serotonin Reuptake Inhibitors (SSRIs): Antidepressants like fluoxetine (Prozac) and sertraline (Zoloft) are often used to treat both anxiety and depression.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Drugs like duloxetine (Cymbalta) help manage anxiety while also targeting chronic pain.
- Buspirone: A non-benzodiazepine anxiolytic that works by modulating serotonin activity.
The Role of Antianxiety Agents in Fibromyalgia Treatment
1. Addressing Emotional Symptoms
Antianxiety agents can help manage the emotional toll of fibromyalgia by reducing stress and promoting a sense of calm. This can indirectly improve other symptoms like pain and fatigue.
2. Enhancing Sleep Quality
Many people with fibromyalgia struggle with insomnia or restless sleep. Some antianxiety medications, particularly benzodiazepines, can help improve sleep by calming the nervous system.
3. Improving Pain Perception
Anxiety can heighten pain perception. By reducing anxiety, antianxiety agents may help patients perceive pain less intensely, making it easier to manage daily activities.
Comparing Antianxiety Agents to Other Fibromyalgia Treatments
1. Medications Targeting Pain
Drugs like pregabalin (Lyrica) and duloxetine (Cymbalta) are FDA-approved for fibromyalgia. While these medications directly target pain and neurological symptoms, antianxiety agents focus more on emotional and psychological well-being.
2. Non-Pharmacological Therapies
Cognitive behavioral therapy (CBT), mindfulness, and physical therapy are effective in addressing both physical and emotional symptoms. However, these approaches require time and effort, while antianxiety agents offer quicker relief.
3. Holistic and Alternative Medicine
Alternative treatments such as yoga, acupuncture, and herbal remedies focus on improving overall well-being. Antianxiety agents can complement these therapies by addressing acute anxiety episodes.
Benefits of Antianxiety Agents for Fibromyalgia
- Rapid Relief: Benzodiazepines provide fast-acting relief for acute anxiety and stress.
- Dual Benefits: SSRIs and SNRIs address both anxiety and other fibromyalgia symptoms, such as pain and depression.
- Improved Quality of Life: Reducing anxiety can enhance social interactions, work performance, and overall daily functioning.
Limitations and Risks of Antianxiety Agents
- Dependency and Tolerance: Long-term use of benzodiazepines carries a risk of dependence and reduced effectiveness.
- Side Effects: Drowsiness, dizziness, and gastrointestinal issues are common side effects of antianxiety medications.
- Not a Cure: Antianxiety agents manage symptoms but do not address the root causes of fibromyalgia or anxiety.
- Need for Comprehensive Treatment: These medications are most effective when used alongside other therapies, such as lifestyle changes and counseling.
Guidelines for Using Antianxiety Agents in Fibromyalgia Management
- Consultation with a Specialist: Always seek advice from a healthcare provider before starting antianxiety medications.
- Short-Term Use: Benzodiazepines should generally be used for short periods to avoid dependence.
- Monitor Side Effects: Report any adverse effects to your doctor to adjust dosages or switch medications.
- Combine with Non-Pharmacological Approaches: Incorporate mindfulness, CBT, and physical activity to maximize benefits.
Real-Life Experiences: How Antianxiety Agents Have Helped
- Emily, 42: Emily started using an SSRI to manage her anxiety and fibromyalgia. Over time, she noticed a reduction in her pain levels and found it easier to sleep.
- James, 50: A combination of buspirone and CBT helped James regain control over his anxiety and improve his daily functioning.
- Sophia, 38: Benzodiazepines provided immediate relief during periods of high stress, helping her manage severe fibromyalgia flare-ups.
Conclusion: Antianxiety Agents as Part of a Comprehensive Fibromyalgia Treatment Plan
While antianxiety agents can play a valuable role in managing the psychological aspects of fibromyalgia, they are not a standalone solution. These medications work best as part of a comprehensive treatment plan that includes lifestyle changes, therapy, and other medical interventions. By addressing anxiety, patients can experience improved quality of life and better control over their fibromyalgia symptoms.
If you’re considering antianxiety agents for fibromyalgia, consult with a healthcare provider to determine the best approach for your unique needs.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores