Introduction
Fibromyalgia is a complex chronic pain condition that affects millions of people worldwide. While widespread pain and fatigue are its hallmark symptoms, sleep disturbances are often an overlooked yet debilitating aspect of the disorder. Many individuals with fibromyalgia struggle with more than just insomnia; hidden sleep disorders can contribute to the severity of their symptoms. Understanding these underlying sleep issues is crucial for managing fibromyalgia effectively.
The Connection Between Fibromyalgia and Sleep
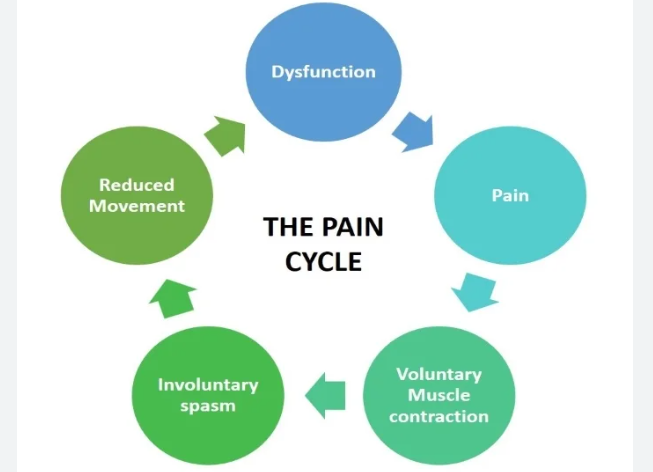
Sleep plays a vital role in the body’s ability to heal and regulate pain. However, people with fibromyalgia often experience disrupted sleep patterns, preventing them from reaching the deep, restorative stages of sleep. This lack of quality sleep exacerbates pain sensitivity, fatigue, and cognitive difficulties, commonly known as fibro fog. The connection between fibromyalgia and sleep disorders suggests that treating sleep disturbances can lead to an overall improvement in symptoms.
Beyond Insomnia: Hidden Sleep Disorders in Fibromyalgia
Although insomnia is a frequent complaint among fibromyalgia patients, several other sleep disorders may go undiagnosed, contributing to their symptoms. Identifying these hidden disorders is key to developing effective treatment strategies.
1. Restless Legs Syndrome (RLS)
Restless Legs Syndrome (RLS) is a neurological disorder that causes uncomfortable sensations in the legs, often leading to an irresistible urge to move them. This condition is particularly common in people with fibromyalgia, disrupting their ability to fall and stay asleep. RLS symptoms are typically worse at night, making it difficult to achieve restorative sleep.
2. Sleep Apnea
Obstructive Sleep Apnea (OSA) is a condition in which breathing repeatedly stops and starts during sleep due to airway obstruction. Many fibromyalgia sufferers may unknowingly experience sleep apnea, leading to fragmented sleep and reduced oxygen levels. This can worsen fatigue, brain fog, and daytime sleepiness, which are already prevalent in fibromyalgia.
3. Alpha-Delta Sleep Anomaly
Individuals with fibromyalgia often exhibit a phenomenon called alpha-delta sleep anomaly, where bursts of wakeful brain activity (alpha waves) intrude into deep sleep stages (delta waves). This disruption prevents the body from experiencing truly restorative sleep, leaving individuals feeling unrefreshed upon waking.
4. Delayed Sleep Phase Syndrome (DSPS)
Delayed Sleep Phase Syndrome (DSPS) is a circadian rhythm disorder in which a person’s sleep-wake cycle is significantly delayed. Those with fibromyalgia and DSPS may find it difficult to fall asleep until the early morning hours, leading to insufficient and poor-quality sleep.
How to Improve Sleep with Fibromyalgia
Managing sleep disturbances in fibromyalgia requires a multi-faceted approach that includes lifestyle changes, sleep hygiene practices, and medical interventions. Here are some strategies that may help improve sleep quality:
1. Establish a Consistent Sleep Schedule
Going to bed and waking up at the same time every day, even on weekends, helps regulate the body’s internal clock and promotes better sleep patterns.
2. Create a Relaxing Bedtime Routine
Engaging in calming activities before bed, such as reading, meditation, or a warm bath, can signal the body that it’s time to wind down and prepare for sleep.
3. Optimize Sleep Environment
A cool, dark, and quiet bedroom can promote restful sleep. Investing in a comfortable mattress and pillows can also help alleviate body pain and discomfort.
4. Address Underlying Sleep Disorders
If symptoms of sleep apnea, RLS, or other disorders are suspected, seeking medical evaluation and appropriate treatment can significantly improve sleep quality.
5. Limit Stimulants and Electronic Devices
Reducing caffeine intake, especially in the afternoon and evening, can prevent sleep disturbances. Additionally, minimizing screen time before bed can reduce exposure to blue light, which can interfere with melatonin production and sleep onset.
Conclusion
Fibromyalgia and sleep disorders are closely intertwined, and addressing sleep disturbances can lead to meaningful improvements in overall well-being. Beyond insomnia, conditions such as restless legs syndrome, sleep apnea, and alpha-delta sleep anomaly can exacerbate fibromyalgia symptoms. By identifying and treating these hidden sleep disorders, individuals with fibromyalgia can achieve better sleep and enhance their quality of life.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores