Fibromyalgia is a complex, chronic condition primarily characterized by widespread pain, fatigue, and sleep disturbances. While the physical symptoms of fibromyalgia are well-known, the emotional and psychological aspects of the disorder are often overlooked. One of the more subtle but impactful manifestations of fibromyalgia is changes in personality. These changes can include shifts in mood, behavior, and cognitive function that may not only affect the individual’s personal life but also their social and professional interactions. In this article, we will explore the connection between fibromyalgia and personality changes, examine the common symptoms, and discuss potential causes and management strategies.
What is Fibromyalgia?
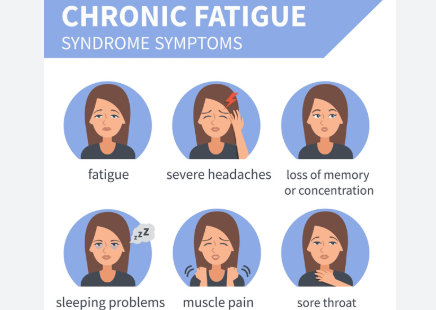
Fibromyalgia is a condition that affects the muscles, ligaments, and tendons, causing chronic pain throughout the body. It is often accompanied by a variety of other symptoms, including fatigue, sleep disturbances, difficulty concentrating (commonly referred to as “fibro fog”), and emotional disturbances. While the exact cause of fibromyalgia remains unclear, it is believed to involve an abnormal response to pain signals and may be influenced by genetic, environmental, and psychological factors. The condition is more common in women and often appears between the ages of 30 and 60, though it can affect individuals of all ages.
Personality Changes in Fibromyalgia: An Overlooked Symptom
Many individuals with fibromyalgia report changes in their behavior, mood, and emotional reactions, which may be perceived as personality shifts. These changes can vary in intensity and may impact relationships, work, and daily functioning. For some, these changes may be gradual and subtle, while for others, they can be more pronounced and disruptive. While not every person with fibromyalgia experiences significant personality changes, those who do may find that their interactions with others and their sense of self are altered.
The personality changes associated with fibromyalgia can often be linked to the emotional and psychological burden of dealing with chronic pain and other symptoms. This strain can lead to heightened stress, anxiety, and depression, which can manifest in shifts in how individuals express their emotions and interact with the world around them.
Common Personality Changes Symptoms in Fibromyalgia
The personality changes that occur in fibromyalgia are complex and multifaceted. Some of the most commonly reported symptoms include:
1. Increased Irritability and Short Temper
One of the most frequent personality changes in fibromyalgia is increased irritability. People with fibromyalgia may find themselves more easily agitated or upset by situations that they would normally handle calmly. This irritability is often linked to the physical discomfort and fatigue that come with chronic pain. The frustration of not feeling well, combined with the inability to predict or manage pain flare-ups, can make individuals more prone to snapping or becoming upset by minor triggers.
2. Social Withdrawal and Isolation
Another common change in personality is social withdrawal. As fibromyalgia causes fatigue, pain, and cognitive issues, individuals may begin to retreat from social situations they once enjoyed. This withdrawal can sometimes be mistaken for disinterest or apathy, but it is often a response to the physical and emotional exhaustion that comes with the condition. The constant struggle with symptoms can make social interactions feel overwhelming, leading to feelings of isolation and detachment.
3. Increased Sensitivity to Stress
People with fibromyalgia often develop a lower tolerance for stress. The chronic nature of the condition means that individuals are constantly dealing with pain, fatigue, and uncertainty about their health. As a result, they may become more easily overwhelmed by everyday stressors. This heightened sensitivity to stress can lead to mood swings and a tendency to react more strongly to challenges or problems.
4. Anxiety and Worry
Anxiety is another common emotional shift that many individuals with fibromyalgia experience. The unpredictability of symptoms, the impact on daily functioning, and the lack of clear answers regarding the cause of the condition can lead to constant worry. This anxiety can alter a person’s personality, making them more anxious, fearful, or hyper-vigilant in everyday situations. For some, anxiety can also lead to an avoidance of certain situations or places that they associate with discomfort or stress.
5. Depression and Feelings of Hopelessness
Depression is frequently reported in individuals with fibromyalgia and can contribute to noticeable personality changes. The ongoing pain and fatigue can lead to feelings of hopelessness, sadness, and loss of interest in previously enjoyed activities. This shift in mood can result in a person becoming more withdrawn, passive, or pessimistic. Depression can also lead to changes in sleep patterns, appetite, and energy levels, all of which can further exacerbate the personality changes associated with fibromyalgia.
6. Difficulty Concentrating and Memory Problems (“Fibro Fog”)
The cognitive symptoms of fibromyalgia, often referred to as “fibro fog,” can also contribute to personality changes. People with fibromyalgia often experience difficulties with concentration, memory, and mental clarity. This cognitive dysfunction can make it challenging to engage in tasks that require focus, which can lead to frustration and irritability. Over time, these cognitive issues can alter the way an individual perceives their abilities, potentially leading to feelings of inadequacy or embarrassment.
7. Heightened Emotional Sensitivity
Individuals with fibromyalgia may experience increased emotional sensitivity, where they feel emotions more intensely than they did before the onset of the condition. Small events may trigger strong emotional reactions, whether positive or negative. This heightened emotional sensitivity can contribute to mood swings, irritability, and difficulty managing feelings of frustration, sadness, or anger.
Potential Causes of Personality Changes in Fibromyalgia
The personality changes experienced by individuals with fibromyalgia are believed to be linked to a variety of factors, including:
1. Chronic Pain and Fatigue
Chronic pain and fatigue are the hallmark symptoms of fibromyalgia, and they can take a significant emotional toll. The constant strain of dealing with pain, along with the mental exhaustion from fatigue, can lead to mood changes and altered behavior. As individuals struggle with their symptoms, they may become more irritable, withdrawn, or anxious, leading to changes in their personality.
2. Sleep Disturbances
Sleep disturbances are common in fibromyalgia and can further exacerbate personality changes. Poor sleep quality and frequent waking throughout the night can result in daytime fatigue, mood swings, and difficulty coping with stress. Chronic sleep deprivation can also impair cognitive function, leading to “fibro fog” and a diminished ability to focus or engage in social interactions.
3. Emotional Stress and Anxiety
The ongoing emotional stress of managing a chronic illness like fibromyalgia can contribute to personality changes. The unpredictability of symptoms, the lack of a definitive diagnosis, and the frustration of feeling misunderstood can all create emotional strain. This stress can manifest as anxiety, depression, irritability, and a heightened sensitivity to stress.
4. Cognitive Dysfunction (“Fibro Fog”)
The cognitive dysfunction associated with fibromyalgia can lead to changes in personality as individuals struggle with memory issues, difficulty concentrating, and mental fatigue. These cognitive challenges can create feelings of confusion or embarrassment, leading to withdrawal or frustration.
5. Chemical Imbalances
Fibromyalgia is believed to involve central nervous system sensitization, which may lead to imbalances in the way the brain processes pain and emotions. These chemical imbalances could contribute to mood swings, irritability, and heightened emotional responses, all of which can alter personality.
Managing Personality Changes in Fibromyalgia
While personality changes can be a challenging aspect of fibromyalgia, there are strategies that individuals can use to manage these shifts and improve emotional well-being:
1. Therapy and Counseling
Cognitive Behavioral Therapy (CBT) and other forms of counseling can be beneficial in helping individuals manage the emotional aspects of fibromyalgia. Therapy can help address negative thought patterns, provide coping strategies for managing stress, and support individuals in improving their mood and emotional responses.
2. Stress Management Techniques
Incorporating stress-reduction techniques such as mindfulness meditation, deep breathing exercises, and progressive muscle relaxation can help individuals with fibromyalgia manage emotional stress. These practices can promote relaxation and emotional stability, helping to reduce irritability and anxiety.
3. Exercise and Physical Activity
Regular physical activity, though challenging for many with fibromyalgia, has been shown to improve mood and reduce stress. Low-impact exercises, such as swimming, walking, or yoga, can help alleviate pain and improve sleep, which in turn may reduce emotional symptoms.
4. Medication
Medications may be prescribed to manage depression, anxiety, and other emotional symptoms associated with fibromyalgia. Antidepressants, anxiolytics, and sleep aids can help regulate mood and improve sleep, which can lead to improvements in personality and overall emotional well-being.
5. Support Networks
Having a support network is crucial for managing personality changes in fibromyalgia. Connecting with others who understand the challenges of living with the condition can provide emotional validation and reduce feelings of isolation. Family, friends, and support groups can help individuals navigate the emotional aspects of fibromyalgia.
Conclusion
Personality changes are a significant yet often overlooked aspect of fibromyalgia. The emotional strain of dealing with chronic pain, fatigue, and other symptoms can lead to shifts in mood, behavior, and cognitive function. While these changes can be challenging, they can be managed with the right strategies, including therapy, stress management, physical activity, and medication. By addressing the emotional aspects of fibromyalgia, individuals can improve their overall quality of life and better navigate the complexities of this chronic condition.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores