Living with fibromyalgia is already a heavy burden. It affects your body, your energy, your mind, and your ability to do things others take for granted. But when the people around you don’t take fibromyalgia seriously, that burden becomes almost unbearable. It’s not just about enduring pain—it’s about carrying the emotional weight of disbelief, invalidation, and silence.
This experience is common among those with invisible illnesses. You are expected to keep up, smile through the fatigue, and explain your condition over and over again to those who still don’t understand. When that effort is met with skepticism or indifference, the damage runs deep.
Here’s what it truly feels like when people don’t take fibromyalgia seriously.
You Start Questioning Your Own Reality
When others downplay your pain, it’s easy to start doubting yourself. You wonder if maybe you are exaggerating. Maybe you should be doing more. Maybe you’re just too sensitive. This internal dialogue doesn’t come from nowhere—it grows out of repeated invalidation.
Over time, the constant second-guessing erodes your confidence in your own body. You stop trusting what you feel, You push through symptoms that need rest. You try to meet expectations that are out of reach. All because someone else made you feel like your illness wasn’t real enough.
The Silence in Conversations Becomes Deafening
When people stop asking how you’re doing, when they change the subject after you mention your pain, or when they avoid talking about your condition altogether—it sends a message. A message that says your experience makes them uncomfortable or that it’s not worth acknowledging.
That silence is louder than words. It creates a barrier between you and the people you care about. It makes every conversation feel like a performance, where you have to pretend you’re okay just to be included.
You Feel Pressure to Look Better Than You Feel
People with fibromyalgia often feel forced to mask their symptoms. You put on makeup to hide the exhaustion, You stand a little taller to appear stronger. You push through activities so no one will call you out for canceling plans.
The irony is that looking well can lead others to believe you’re not sick, which only deepens the cycle of disbelief. It becomes a game you can’t win. Show your pain, and you’re seen as dramatic. Hide it, and you’re not believed.
You Carry Guilt That Shouldn’t Be Yours
When others don’t take your illness seriously, you end up carrying guilt for things that are beyond your control. You feel bad for canceling, You feel guilty for needing rest. You apologize for missing events or not returning calls quickly.
But fibromyalgia isn’t your fault. The guilt doesn’t belong to you. It belongs to a culture that struggles to accept chronic illness, especially when it can’t be seen or cured.
You Stop Talking About It Altogether
Eventually, many people with fibromyalgia stop trying to explain. They stop sharing. They keep their pain to themselves because experience has taught them that honesty often leads to dismissal. This silence isn’t healing—it’s self-protection.
But that silence also leads to isolation. You feel alone in your experience, even when surrounded by others. That’s one of the most painful parts of being dismissed—not just feeling misunderstood, but feeling unseen.
You Begin to Grieve the Support You Never Received
When people don’t take fibromyalgia seriously, it’s not just disappointing—it’s a form of loss. You grieve the support you hoped to receive from friends, family, coworkers, or doctors. You grieve the connection that was supposed to come from understanding and compassion.
This grief doesn’t always come with tears. Sometimes it comes as numbness, withdrawal, or the quiet acceptance that you have to face this journey on your own.
Frequently Asked Questions
1. Why don’t people take fibromyalgia seriously?
Because it’s an invisible illness with no definitive tests, and because it’s often misunderstood by the public and even some medical professionals. Stigma and misinformation contribute to disbelief.
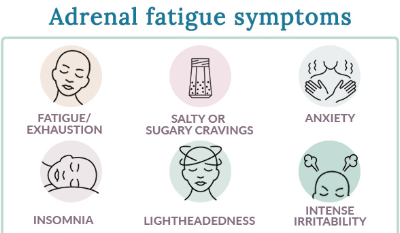
2. How does disbelief affect someone with fibromyalgia emotionally?
It leads to self-doubt, anxiety, depression, isolation, and a loss of trust in relationships and healthcare systems.
3. What should you say to someone who shares they have fibromyalgia?
Say “I believe you.” Ask how you can support them. Avoid offering solutions unless asked. Just listening can mean everything.
4. How can I explain my illness to someone who doesn’t understand?
Use clear, simple language. Share specific symptoms and how they affect your daily life. If they still don’t listen, know that you’re not responsible for their understanding.
5. Is it okay to distance yourself from unsupportive people?
Yes. Protecting your emotional and physical health is valid. Surround yourself with those who show empathy and respect.
6. Can society improve how it sees fibromyalgia?
Yes, through awareness, education, and listening to people with lived experience. As more voices speak out, stigma can be replaced with understanding.
What it feels like when people don’t take fibromyalgia seriously isn’t just frustration—it’s heartbreak. It’s the pain of being unheard, the exhaustion of having to explain, and the loneliness of knowing your suffering is invisible to those who matter most. But your experience is real. Your voice matters. And even if others don’t see it, your strength is undeniable. Keep speaking. Keep honoring your truth. Because you deserve to be believed.
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores