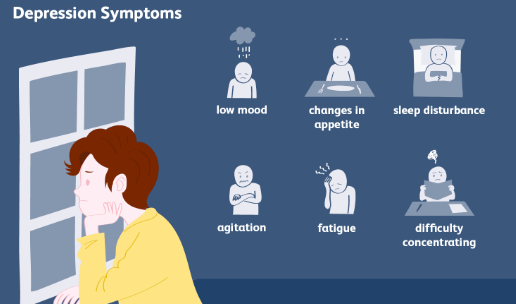
Fibromyalgia is a chronic condition that primarily affects the muscles and joints, leading to widespread pain, fatigue, and sleep disturbances. While its hallmark symptoms are well-known, there are several lesser-recognized manifestations of the condition that can significantly impact the quality of life. One such issue that is not often discussed is hearing loss or related auditory symptoms. In this article, we will explore the potential link between fibromyalgia and hearing loss, identify common symptoms, and discuss possible causes and treatment strategies.
Understanding Fibromyalgia
Fibromyalgia is a disorder characterized by widespread musculoskeletal pain, fatigue, and sleep disturbances. The exact cause of fibromyalgia is still unknown, but researchers believe it may be linked to an abnormal response to pain signals in the brain and nervous system. While it is often associated with joint and muscle pain, fibromyalgia can affect various bodily systems, leading to symptoms that go beyond the commonly known ones, such as hearing loss.
The Link Between Fibromyalgia and Hearing Loss
Although hearing loss is not typically classified as a core symptom of fibromyalgia, there is increasing evidence that suggests a connection between the two. Some individuals with fibromyalgia report experiencing auditory symptoms such as tinnitus (ringing in the ears), difficulty hearing certain frequencies, or a sensation of fullness in the ears. These auditory disturbances may be linked to the overall nervous system dysfunction present in fibromyalgia patients.
Nervous System Sensitivity
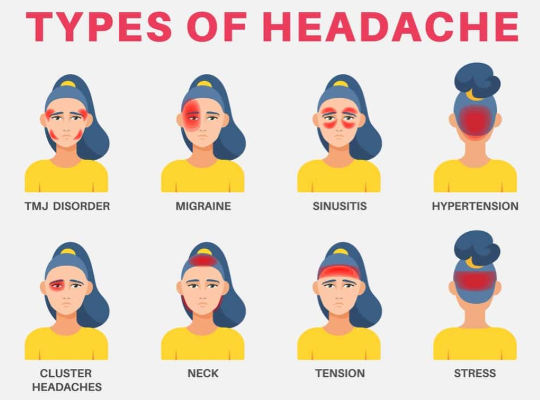
Fibromyalgia is often associated with heightened sensitivity in the nervous system, a phenomenon known as central sensitization. In individuals with central sensitization, the brain amplifies sensory signals, including pain, sounds, and other sensations. This sensitivity can lead to auditory disturbances, as the brain may misinterpret or overreact to normal sounds. This hypersensitivity could contribute to tinnitus or the sensation of muffled hearing.
Autonomic Nervous System Dysfunction
The autonomic nervous system, which controls involuntary functions such as heart rate and blood pressure, may also play a role in the auditory symptoms experienced by people with fibromyalgia. Dysfunction in this system can cause irregularities in blood flow to the ears, leading to symptoms like ear fullness, dizziness, or even hearing problems. Additionally, fibromyalgia can cause changes in blood pressure regulation, which may contribute to fluctuations in ear pressure and hearing.
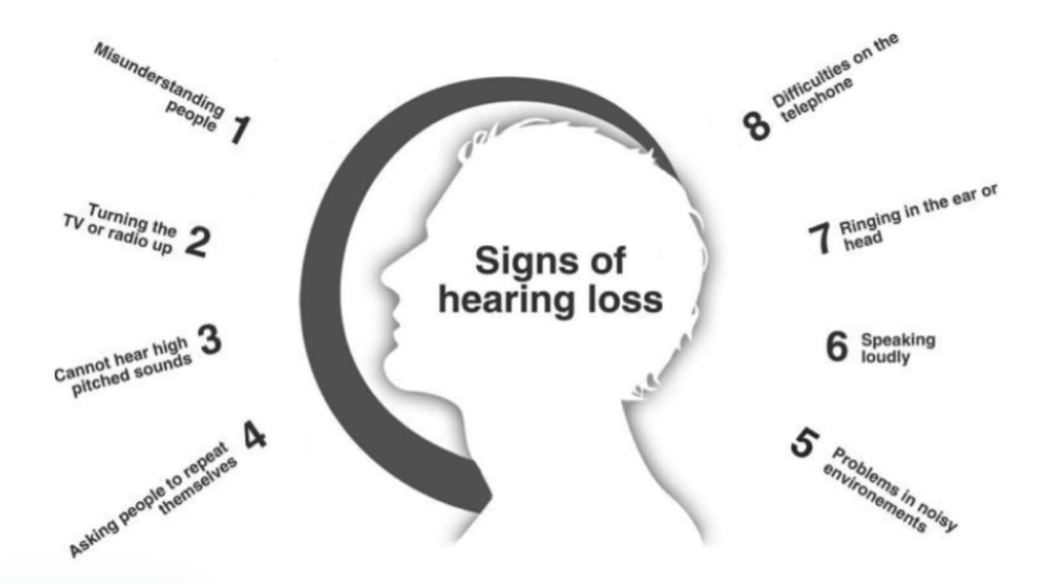
Common Hearing Loss Symptoms in Fibromyalgia
While fibromyalgia-related hearing loss is not always recognized, many people with the condition experience auditory symptoms that are consistent with hearing issues. These symptoms may include:
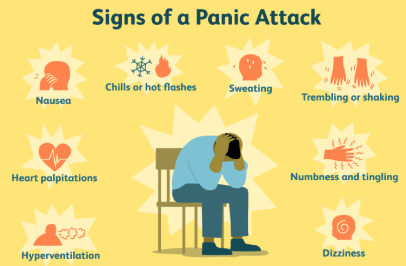
- Tinnitus (Ringing in the Ears): One of the most commonly reported auditory symptoms in fibromyalgia patients is tinnitus. This condition causes a persistent ringing, buzzing, or hissing sound in the ears, which can be constant or intermittent. Tinnitus can significantly impact daily life and sleep quality.
- Difficulty Hearing Certain Frequencies: Some individuals with fibromyalgia report a diminished ability to hear certain high or low frequencies. This may manifest as trouble understanding speech in noisy environments or difficulty hearing high-pitched sounds, such as a telephone ringing or a bird chirping.
- Ear Fullness or Pressure: A sensation of fullness or pressure in the ears is another symptom that can occur in individuals with fibromyalgia. This feeling may resemble the sensation of having clogged ears or being on an airplane and can cause discomfort or difficulty hearing clearly.
- Hyperacusis (Sensitivity to Sound): People with fibromyalgia may develop hyperacusis, a condition in which everyday sounds seem overly loud or uncomfortable. This heightened sensitivity to sound can contribute to auditory distress and discomfort in otherwise quiet environments.
Potential Causes of Hearing Loss in Fibromyalgia
The exact reasons why hearing loss or auditory disturbances occur in fibromyalgia are not fully understood. However, several factors may contribute to these symptoms:
Central Nervous System Dysfunction
Fibromyalgia is believed to involve dysfunction in the central nervous system, which may affect the way the brain processes sensory information. This dysfunction can cause a heightened sensitivity to sound and other sensory stimuli, leading to conditions like tinnitus and hyperacusis.
Inflammation and Blood Flow Issues
Fibromyalgia is also associated with increased levels of inflammation in the body. Chronic inflammation may affect blood vessels, leading to poor circulation in various parts of the body, including the ears. Reduced blood flow to the auditory system can contribute to hearing disturbances and ear-related symptoms.
Medication Side Effects
Many individuals with fibromyalgia take medications to manage their symptoms, including pain relievers, antidepressants, and anti-seizure drugs. Some of these medications can have side effects that affect hearing or cause auditory disturbances. For example, certain medications may cause tinnitus, dizziness, or a sensation of fullness in the ears.
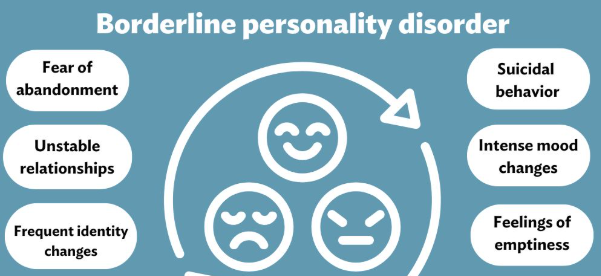
Stress and Anxiety
Stress and anxiety are common among people with fibromyalgia, and they can exacerbate a range of symptoms, including auditory issues. High stress levels can lead to increased tension in the body, which may contribute to the development of tinnitus or make existing auditory symptoms worse.
Diagnosing Hearing Loss in Fibromyalgia
Diagnosing hearing loss in individuals with fibromyalgia can be challenging because the auditory symptoms may overlap with other conditions or be mistaken for normal age-related hearing loss. A thorough evaluation by a healthcare professional is necessary to determine whether the hearing issues are related to fibromyalgia or another underlying condition.
A hearing test (audiometry) is typically used to assess the level of hearing loss and identify any specific frequencies that may be affected. In some cases, additional tests such as MRI scans or CT scans may be performed to rule out other possible causes of hearing loss, such as ear infections or damage to the auditory nerves.
Managing Hearing Loss Symptoms in Fibromyalgia
While there is no cure for fibromyalgia or its associated auditory symptoms, there are several strategies that individuals can use to manage hearing loss and related symptoms effectively.
Tinnitus Management
For those experiencing tinnitus, various treatments can help reduce the severity of the ringing in the ears. Cognitive behavioral therapy (CBT) is a common approach used to help patients manage the emotional distress caused by tinnitus. Sound therapy, which involves using white noise or background sounds to mask the ringing, can also be helpful in alleviating the discomfort of tinnitus.
Stress Reduction Techniques
Since stress is a known trigger for both fibromyalgia and hearing loss symptoms, incorporating stress reduction techniques such as meditation, deep breathing exercises, and yoga can be beneficial in managing auditory disturbances. Reducing stress may help decrease the intensity of symptoms like tinnitus and hyperacusis.
Hearing Aids and Sound Amplifiers
For individuals with significant hearing loss, hearing aids or sound amplifiers may be recommended. These devices can help amplify certain frequencies and improve communication in social settings. Additionally, assistive listening devices can be used to reduce the impact of background noise, making it easier to hear conversations.
Medication Adjustments
If medication side effects are contributing to hearing issues, a healthcare provider may adjust the treatment regimen or prescribe alternative medications to reduce auditory disturbances. It is important to work closely with a doctor to ensure that both fibromyalgia and hearing-related symptoms are properly managed.
Conclusion
Hearing loss symptoms in fibromyalgia, although less commonly discussed, can significantly impact the lives of individuals living with the condition. Whether through tinnitus, difficulty hearing certain frequencies, or sensitivity to sound, these auditory disturbances can add another layer of complexity to an already challenging illness. Understanding the potential link between fibromyalgia and hearing loss, as well as implementing appropriate management strategies, can help improve the quality of life for those affected by both conditions.
By working with healthcare providers to address both the physical and auditory symptoms of fibromyalgia, individuals can take proactive steps toward managing their health and well-being.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores