Fibromyalgia is a chronic condition characterized by widespread pain, fatigue, and cognitive issues, with symptoms often extending to various bodily systems. While musculoskeletal pain and fatigue are the hallmark features of fibromyalgia, gastrointestinal issues, including heartburn, are increasingly recognized as common symptoms among those affected by this disorder. Heartburn, a sensation of burning in the chest caused by acid reflux, may seem unrelated to fibromyalgia at first glance, but a closer look reveals a complex interplay between the two conditions. In this article, we will explore how heartburn presents in fibromyalgia, its potential causes, and strategies for managing it.
Understanding Heartburn and Fibromyalgia
Heartburn, also known as acid reflux, occurs when stomach acid flows backward into the esophagus, causing irritation and the characteristic burning sensation in the chest. This can be caused by various factors, including diet, stress, and anatomical issues like a weakened lower esophageal sphincter (LES). Chronic heartburn is commonly associated with gastroesophageal reflux disease (GERD), a condition that can lead to more severe complications if left untreated.
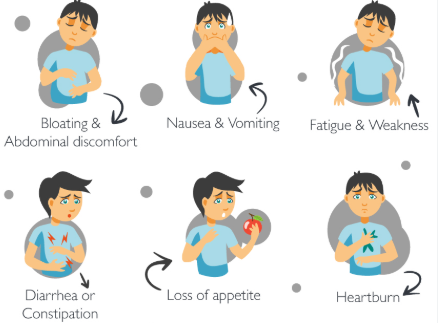
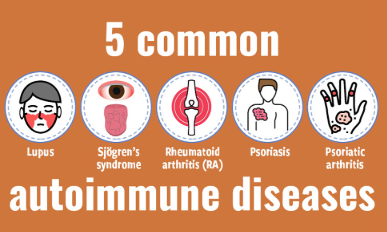
On the other hand, fibromyalgia is a complex and poorly understood condition that primarily causes chronic musculoskeletal pain, fatigue, and sleep disturbances. Though fibromyalgia is generally not thought of as a digestive disorder, many individuals with fibromyalgia report experiencing gastrointestinal symptoms, including heartburn. These gastrointestinal issues are often overlooked in clinical practice, leading to a lack of awareness regarding their impact on patients’ overall health.
The Link Between Heartburn and Fibromyalgia
While heartburn and fibromyalgia are distinct conditions, there is growing evidence to suggest a connection between the two. The exact mechanisms behind this link are not fully understood, but several factors may contribute to the co-occurrence of heartburn and fibromyalgia:
1. Increased Sensitivity to Pain
One of the hallmark features of fibromyalgia is central sensitization, a phenomenon in which the nervous system becomes hypersensitive to pain signals. This heightened sensitivity can make individuals with fibromyalgia more prone to experiencing discomfort from everyday sensations, such as the acid reflux associated with heartburn. In people with fibromyalgia, the pain caused by heartburn may feel more intense or distressing than it would in those without the condition.
2. Stress and Anxiety
Stress and anxiety are prevalent in individuals with fibromyalgia, as they can exacerbate both pain and fatigue. Emotional distress can also trigger physical symptoms, including gastrointestinal issues like heartburn. Chronic stress can increase stomach acid production and weaken the LES, leading to an increased likelihood of acid reflux. This creates a vicious cycle where stress triggers heartburn, which in turn worsens the overall symptoms of fibromyalgia.
3. Medications Used for Fibromyalgia
Many individuals with fibromyalgia take medications to manage pain and other symptoms, such as antidepressants, anticonvulsants, and pain relievers. Some of these medications, particularly NSAIDs (nonsteroidal anti-inflammatory drugs), can irritate the stomach lining, leading to heartburn or acid reflux. In addition, medications that affect the central nervous system can influence the digestive process, potentially increasing the risk of gastrointestinal issues, including heartburn.
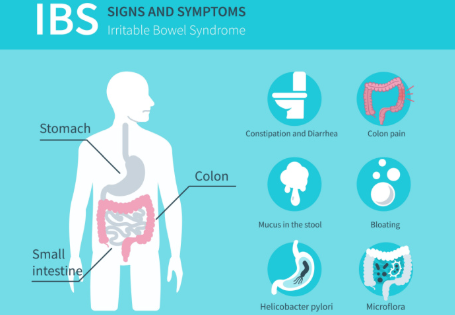
4. Gastrointestinal Motility Issues
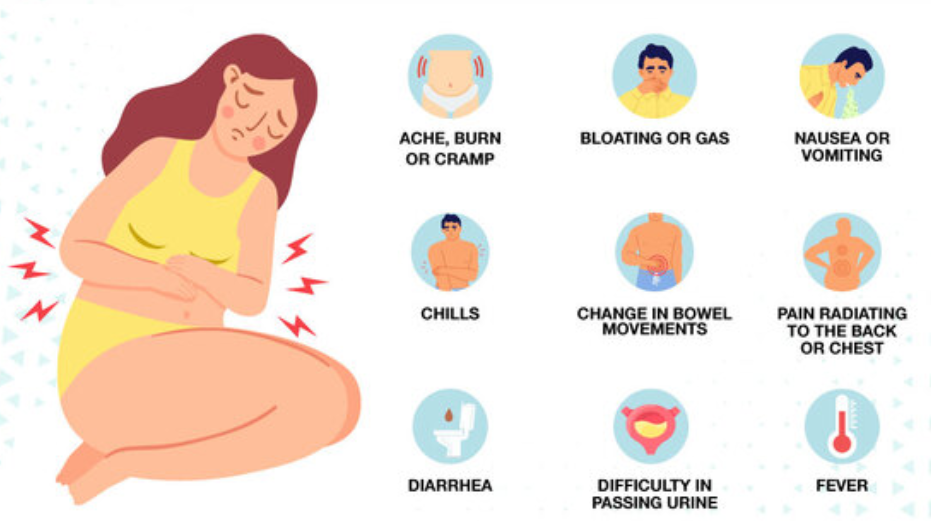
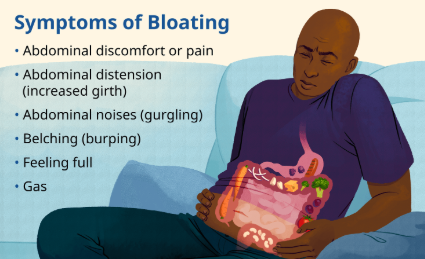
Some individuals with fibromyalgia experience gastrointestinal dysmotility, which refers to the disruption of normal digestive movements. This can lead to slower digestion, bloating, and delayed gastric emptying. The slowed digestive process can contribute to an increase in stomach acid, leading to acid reflux and heartburn symptoms. The disruption in gastrointestinal motility is thought to be related to the abnormal processing of pain and discomfort that is characteristic of fibromyalgia.
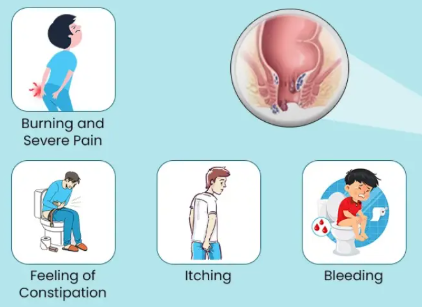
Common Symptoms of Heartburn in Fibromyalgia
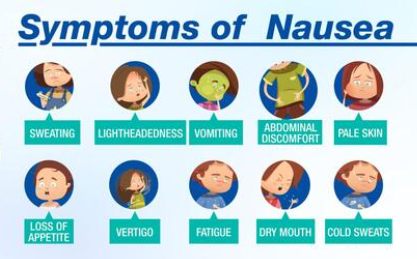
Individuals with fibromyalgia who also experience heartburn may have a range of overlapping symptoms. These symptoms can vary in intensity and frequency but generally include the following:
1. Burning Sensation in the Chest
The hallmark symptom of heartburn is a burning sensation in the chest, often referred to as acid indigestion. This sensation typically occurs after eating, especially after consuming foods that are spicy, fatty, or acidic. The burning may worsen when lying down or bending over.
How it affects fibromyalgia: For those with fibromyalgia, the intensity of the burning sensation may feel more pronounced due to the heightened pain sensitivity associated with the condition. This can exacerbate the discomfort and stress associated with fibromyalgia.
2. Regurgitation of Acidic Fluid
Another common symptom of heartburn is the regurgitation of acidic fluid into the mouth or throat. This can lead to a sour or bitter taste and a feeling of food coming back up. Regurgitation may occur, especially when lying down or after large meals.
How it affects fibromyalgia: In fibromyalgia patients, the regurgitation of acid can cause additional discomfort and contribute to the overall sense of gastrointestinal distress. This symptom may also disrupt sleep, which is already a major issue for many individuals with fibromyalgia.
3. Difficulty Swallowing
Some individuals with heartburn may experience dysphagia, or difficulty swallowing, which can occur when stomach acid irritates the esophagus. This can make swallowing food or liquids feel uncomfortable or even painful.
How it affects fibromyalgia: Difficulty swallowing can contribute to feelings of anxiety and frustration, further complicating the cognitive and emotional symptoms of fibromyalgia. The discomfort can also disrupt daily life and eating habits.
4. Hoarseness or Sore Throat
When acid from the stomach reaches the throat, it can cause irritation and inflammation, leading to hoarseness or a sore throat. This is commonly referred to as laryngopharyngeal reflux (LPR) and can be especially bothersome for fibromyalgia patients, as it adds to their existing symptoms of fatigue and pain.
How it affects fibromyalgia: Chronic throat irritation can disrupt communication, lead to a feeling of constant discomfort, and interfere with sleep—adding another layer to the already complex symptomatology of fibromyalgia.
5. Persistent Cough
In some cases, heartburn can cause a chronic cough, especially when stomach acid irritates the airways. This symptom is more common at night and can disrupt sleep.
How it affects fibromyalgia: Sleep disturbances are a major concern for individuals with fibromyalgia. A persistent cough that interferes with sleep can worsen fatigue, cognitive dysfunction, and overall pain, leading to a more challenging experience for individuals dealing with both conditions.
Managing Heartburn Symptoms in Fibromyalgia
Managing heartburn symptoms in individuals with fibromyalgia requires a comprehensive approach that addresses both the digestive issues and the underlying fibromyalgia symptoms. Here are several strategies for managing heartburn in the context of fibromyalgia:
1. Dietary Adjustments
Certain foods are known to trigger heartburn, including spicy foods, citrus, tomatoes, chocolate, and fatty foods. Making dietary changes to avoid these triggers can help alleviate heartburn symptoms. Additionally, eating smaller meals and avoiding large meals before bedtime can reduce the risk of acid reflux.
For fibromyalgia: A diet that is rich in anti-inflammatory foods—such as leafy greens, fruits, whole grains, and lean proteins—can support overall health and may help reduce fibromyalgia symptoms as well.
2. Stress Management Techniques
Since stress is a significant trigger for both heartburn and fibromyalgia, incorporating stress management techniques such as deep breathing, meditation, yoga, or mindfulness can help reduce both gastrointestinal and fibromyalgia symptoms.
For fibromyalgia: Stress reduction is key to managing fibromyalgia flare-ups, as emotional distress can exacerbate pain and fatigue. Finding healthy coping mechanisms for stress is essential for improving overall well-being.
3. Medication Management
For individuals with fibromyalgia, careful consideration of the medications they are taking is important. If NSAIDs or other medications are contributing to heartburn, healthcare providers may suggest alternative treatments or recommend acid-suppressing medications, such as antacids, proton pump inhibitors (PPIs), or H2 blockers.
For fibromyalgia: Pain management medications that do not exacerbate gastrointestinal symptoms should be prioritized. A combination of medications that addresses both fibromyalgia pain and heartburn can provide more effective relief.
4. Lifestyle Modifications
Adopting lifestyle modifications, such as elevating the head of the bed, avoiding lying down immediately after meals, and maintaining a healthy weight, can help reduce heartburn symptoms. Regular physical activity, which is beneficial for managing fibromyalgia, can also support digestive health and help alleviate stress.
Conclusion
Heartburn is a common yet often underrecognized symptom in individuals with fibromyalgia. The interplay between fibromyalgia and heartburn is complex, with factors such as stress, medications, and increased pain sensitivity contributing to the development of gastrointestinal issues. By understanding the connection between the two conditions and implementing strategies such as dietary changes, stress management, and proper medication, individuals can better manage both their fibromyalgia and heartburn symptoms, improving their quality of life and overall health.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores