Living with fibromyalgia can be overwhelming due to its widespread pain, fatigue, and challenges in maintaining daily activities. While medications, lifestyle changes, and holistic approaches are often recommended, physical therapy stands out as a vital treatment option. But how does physical therapy fare against fibromyalgia symptoms? Can it truly make a difference in managing this chronic condition? Let’s explore the role of physical therapy in tackling fibromyalgia and its potential benefits.
What is Fibromyalgia?
Fibromyalgia is a chronic condition that causes widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive difficulties (often called “fibro fog“). While the exact cause of fibromyalgia remains unclear, it is thought to involve abnormal pain processing in the central nervous system, heightened sensitivity to pain stimuli, and potential contributions from genetics, stress, or trauma.
Since fibromyalgia affects not only physical health but also emotional well-being, a multidisciplinary approach to treatment is often essential. This is where physical therapy can play a critical role.
The Role of Physical Therapy in Fibromyalgia Management
Understanding Physical Therapy
Physical therapy (PT) involves guided exercises, manual techniques, and patient education designed to improve mobility, reduce pain, and restore function. For individuals with fibromyalgia, PT focuses on developing gentle, low-impact interventions that accommodate the heightened pain sensitivity associated with the condition.
How Physical Therapy Helps Fibromyalgia
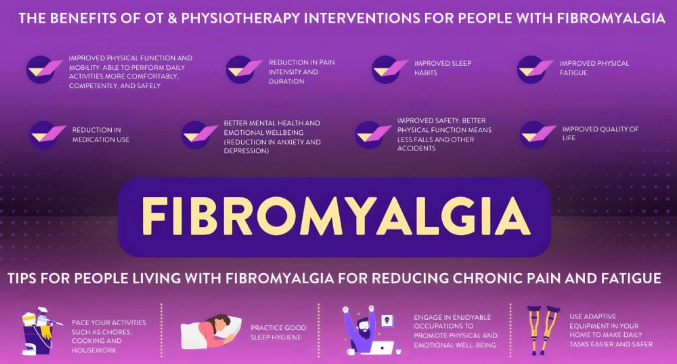
Physical therapy offers several benefits for fibromyalgia patients, including:
- Pain Management: Specific techniques can reduce localized pain and help desensitize the nervous system.
- Improved Flexibility and Mobility: Exercises target stiff muscles and joints, enhancing range of motion.
- Reduced Fatigue: Gradual, structured movement can improve energy levels and reduce the sense of exhaustion.
- Stress Reduction: Physical therapy often includes relaxation techniques that alleviate stress, a known trigger for fibromyalgia symptoms.
Physical Therapy Techniques for Fibromyalgia
1. Stretching Exercises
Gentle stretching exercises are foundational in physical therapy for fibromyalgia. They help alleviate muscle tightness, improve flexibility, and promote relaxation. Examples include yoga-inspired stretches and light dynamic movements tailored to the individual.
2. Aerobic Conditioning
Low-impact aerobic exercises such as walking, swimming, or cycling can improve cardiovascular health while reducing pain and fatigue over time. Physical therapists guide patients in starting slow and gradually increasing activity to avoid symptom flares.
3. Strength Training
Building muscle strength helps support joints and improves overall function. Therapists design fibromyalgia-friendly routines using light weights, resistance bands, or bodyweight exercises.
4. Manual Therapy
Hands-on techniques like myofascial release, massage, and trigger point therapy can alleviate muscle tension, improve circulation, and address localized pain points.
5. Hydrotherapy
Water-based exercises are particularly beneficial for fibromyalgia patients. The buoyancy of water reduces strain on joints, allowing for easier movement while still building strength and flexibility.
6. Posture Training
Improving posture reduces strain on muscles and joints, alleviating pain and promoting long-term physical health.
Benefits of Physical Therapy for Fibromyalgia Patients
Physical therapy offers tailored solutions for the unique challenges of fibromyalgia. Key benefits include:
1. Personalized Care
Every fibromyalgia case is different. A skilled physical therapist can assess individual symptoms and create a customized program.
2. Non-Invasive and Drug-Free
Physical therapy is a natural alternative to medications, making it a great option for individuals seeking non-pharmacological pain relief.
3. Improved Functionality
Patients often report improved ability to perform daily activities, thanks to better mobility and reduced stiffness.
4. Empowerment and Education
Therapists educate patients about body mechanics, proper posture, and self-care techniques, giving them tools to manage symptoms at home.
Limitations of Physical Therapy for Fibromyalgia
While physical therapy is highly beneficial, it is not a standalone solution for fibromyalgia. Patients may encounter some challenges:
- Initial Discomfort: Starting physical therapy can be intimidating, especially for those experiencing severe pain.
- Consistency Needed: Regular sessions are necessary to see lasting results, which can be a challenge for those with fluctuating symptoms.
- Complementary Care Required: Physical therapy works best when combined with other treatments like medication, counseling, and lifestyle changes.
How Physical Therapy Compares to Other Treatments for Fibromyalgia
1. Physical Therapy vs Medications
Medications like pregabalin, duloxetine, or analgesics target pain and mood disorders. Physical therapy, on the other hand, focuses on restoring physical function and addressing the root causes of muscle pain and stiffness.
2. Physical Therapy vs Cognitive Behavioral Therapy (CBT)
While CBT addresses the psychological aspects of fibromyalgia, physical therapy focuses on the physical symptoms. Together, they form a complementary treatment plan.
3. Physical Therapy vs Exercise Alone
While general exercise can benefit fibromyalgia patients, physical therapy provides supervised, individualized programs that minimize the risk of overexertion or injury.
Tips for Maximizing Physical Therapy Benefits
If you’re considering physical therapy for fibromyalgia, here are some tips to maximize its effectiveness:
- Communicate Openly: Let your therapist know about your pain levels, limitations, and goals.
- Be Patient: Progress may be gradual, so don’t get discouraged by slow improvements.
- Commit to Consistency: Regular sessions and at-home exercises are key to achieving results.
- Integrate with Other Therapies: Pair physical therapy with stress management, nutrition, and medication as needed.
Conclusion: Physical Therapy as a Key Player in Fibromyalgia Treatment
Physical therapy is a cornerstone of fibromyalgia care, offering a holistic, non-invasive way to manage pain, improve mobility, and regain quality of life. By addressing both physical and emotional aspects of the condition, it provides a pathway to better health and empowerment.
While physical therapy alone may not “cure” fibromyalgia, it serves as a valuable tool in a comprehensive treatment plan. If you’re living with fibromyalgia, consulting a licensed physical therapist could be the first step toward a more comfortable and active life.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores