Introduction
Fibromyalgia is a chronic condition characterized by widespread pain, fatigue, and a variety of other debilitating symptoms. Understanding its prevalence and impact is crucial for improving diagnosis, treatment, and patient care. This blog post explores the prevalence of fibromyalgia based on a comprehensive survey conducted in five European countries, highlighting the condition’s impact on daily life and discussing the implications for healthcare systems.
Understanding Fibromyalgia
What is Fibromyalgia?
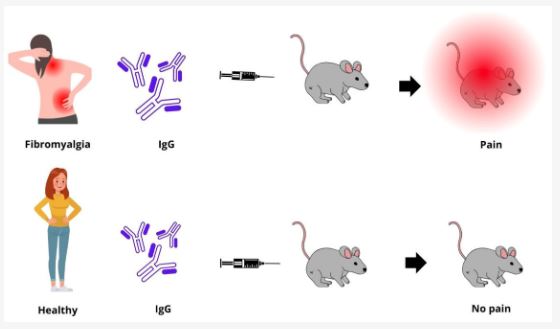
Fibromyalgia is a chronic disorder marked by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive issues. The exact cause of fibromyalgia remains unclear, but it is believed to involve a combination of genetic, environmental, and psychological factors.
Common Symptoms
- Widespread Pain: Persistent pain affecting multiple areas of the body.
- Fatigue: Chronic tiredness that does not improve with rest.
- Sleep Disturbances: Difficulty falling asleep, staying asleep, or achieving restorative sleep.
- Cognitive Issues: Problems with memory, attention, and concentration, often referred to as “fibro fog.”
- Other Symptoms: Headaches, irritable bowel syndrome, and mood disorders such as anxiety and depression.
Click Here to Visit the Store and find Much More….
The Survey: Methodology and Scope
Survey Objectives
The survey aimed to assess the prevalence of fibromyalgia in five European countries, identify common symptoms, and understand the condition’s impact on daily life.
Countries Surveyed
The survey was conducted in the following five European countries:
- United Kingdom
- Germany
- France
- Spain
- Italy
Methodology
The survey utilized a standardized questionnaire to collect data from a representative sample of the population in each country. Participants were asked about their fibromyalgia diagnosis, symptoms, and the impact on their daily lives.
Prevalence of Fibromyalgia: Key Findings
Overall Prevalence
The survey revealed that the prevalence of fibromyalgia varied across the five countries. On average, fibromyalgia affected approximately 2-4% of the adult population in these countries, consistent with global prevalence estimates.
Country-Specific Prevalence
- United Kingdom: Approximately 2.5% of the adult population reported having fibromyalgia.
- Germany: Around 3.2% of adults were diagnosed with fibromyalgia.
- France: The prevalence was estimated at 2.8% of the adult population.
- Spain: About 3.7% of adults reported having fibromyalgia.
- Italy: The prevalence was approximately 3.0% among adults.
Demographic Variations
The survey indicated that fibromyalgia was more common in women than men, with a female-to-male ratio of about 7:1. The condition was also more prevalent in middle-aged and older adults, particularly those aged 40-60 years.
Impact on Daily Life
Work and Employment
Fibromyalgia significantly affected respondents’ ability to work. Many reported reducing their working hours or leaving their jobs entirely due to pain and fatigue. The survey found that 60% of respondents faced employment challenges, impacting their financial stability and quality of life.
Social and Family Life
The condition also had a profound impact on social and family life. About 70% of respondents reported difficulty participating in social activities, and 55% said that fibromyalgia had strained their relationships with family and friends. The chronic pain and fatigue limited their ability to engage in social interactions and maintain meaningful relationships.
Emotional Well-being
The survey highlighted the emotional toll of fibromyalgia. A majority of respondents experienced feelings of frustration, helplessness, and isolation. The chronic nature of the condition and its impact on daily life contributed to these emotional challenges. Anxiety and depression were commonly reported, further exacerbating the overall burden of fibromyalgia.
Click Here to Visit the Store and find Much More….
Healthcare Implications
Diagnosis and Treatment
The survey underscored the need for improved diagnosis and treatment of fibromyalgia. Many respondents reported delays in diagnosis and a lack of effective treatment options. This highlights the importance of raising awareness among healthcare providers and improving diagnostic criteria to ensure timely and accurate identification of fibromyalgia.
Integrated Care Approaches
Given the multifaceted nature of fibromyalgia, integrated care approaches are essential for effective management. This includes a combination of pharmacological treatments, lifestyle changes, psychological support, and alternative therapies. Multidisciplinary care teams can provide comprehensive and personalized treatment plans to address the diverse needs of fibromyalgia patients.
Patient Education and Support
Educating patients about fibromyalgia and providing support resources is crucial for effective self-management. Support groups, educational materials, and counseling services can help patients understand their condition, develop coping strategies, and connect with others facing similar challenges.
Future Directions
Research and Innovation
Ongoing research is vital to advancing our understanding of fibromyalgia and developing new treatment options. Continued studies on the underlying mechanisms, genetic factors, and potential biomarkers can lead to more effective and targeted therapies.
Policy and Advocacy
Advocacy efforts are needed to raise awareness about fibromyalgia and promote policies that support patients. This includes ensuring access to healthcare services, funding for research, and protection of patients’ rights in the workplace and beyond.
FAQs
What is the average prevalence of fibromyalgia in the five European countries surveyed?
The average prevalence of fibromyalgia in the five European countries surveyed (United Kingdom, Germany, France, Spain, and Italy) is approximately 2-4% of the adult population.
Which demographic groups are most affected by fibromyalgia?
Fibromyalgia is more common in women than men, with a female-to-male ratio of about 7:1. It is also more prevalent in middle-aged and older adults, particularly those aged 40-60 years.
How does fibromyalgia impact work and employment?
Fibromyalgia significantly affects work and employment, with many patients reducing their working hours or leaving their jobs entirely due to pain and fatigue. This impacts their financial stability and quality of life.
What are the emotional effects of fibromyalgia?
The emotional effects of fibromyalgia include feelings of frustration, helplessness, isolation, anxiety, and depression. The chronic pain and impact on daily life contribute to these emotional challenges.
What are the key healthcare implications of the survey findings?
The survey highlights the need for improved diagnosis, integrated care approaches, and patient education and support. Raising awareness among healthcare providers and developing comprehensive treatment plans are essential for effective management.
What future directions are important for fibromyalgia research and advocacy?
Future directions include ongoing research to advance understanding and treatment of fibromyalgia, and advocacy efforts to raise awareness, promote policies that support patients, and ensure access to healthcare services.
Conclusion
The survey on the prevalence of fibromyalgia in five European countries provides valuable insights into the condition’s impact on daily life and the need for improved healthcare strategies. By understanding the challenges faced by fibromyalgia patients, healthcare providers can develop more effective and personalized treatment plans. Continued research and advocacy are essential to enhance the quality of life for those living with fibromyalgia and ensure they receive the support and care they need.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores