Introduction: Can Fibromyalgia Be Reversed?
Fibromyalgia is a chronic pain disorder that affects millions worldwide, causing widespread pain, fatigue, and cognitive difficulties. Traditional treatments, including pain medications, physical therapy, and lifestyle adjustments, often provide only partial relief.
However, a new approach known as the Fibromyalgia Reversal Protocol is gaining attention. This protocol focuses on identifying and addressing the root causes of fibromyalgia rather than just managing symptoms. By making strategic changes in diet, lifestyle, and nervous system regulation, many people report significant reductions in pain, increased energy, and improved quality of life.
This article explores the key principles of the Fibromyalgia Reversal Protocol, how it works, and the steps needed to regain control over your health.
Understanding the Fibromyalgia Puzzle: Why Reversal Is Possible
Fibromyalgia is often considered incurable, but emerging research suggests that it is not a permanent condition. Instead, fibromyalgia may be the result of multiple imbalances in the body, including:
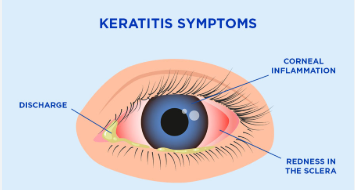
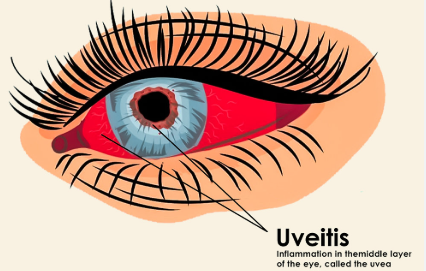
- Chronic inflammation
- Nervous system dysregulation
- Mitochondrial dysfunction (poor energy production at the cellular level)
- Gut health imbalances and leaky gut syndrome
- Hormonal and adrenal dysfunction
By addressing these root causes, it is possible to reduce symptoms, regain energy, and restore normal function.
The Fibromyalgia Reversal Protocol: Key Steps for Healing
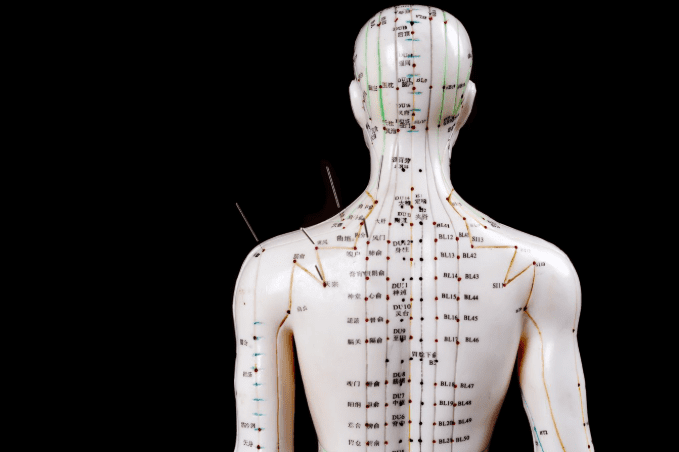
1. Reset the Nervous System to Reduce Pain Sensitivity
Fibromyalgia is often linked to an overactive nervous system, causing hypersensitivity to pain, stress, and sensory input. Rebalancing the nervous system is crucial for reducing pain perception and restoring calm.
Steps to reset the nervous system:
- Vagus nerve stimulation (deep breathing, cold exposure, humming exercises)
- Meditation and mindfulness to calm the brain’s pain response
- Low-dose naltrexone (LDN), a medication that can help modulate pain signals
- Somatic therapy or gentle bodywork (yoga, tai chi, or Feldenkrais method)
2. Reduce Chronic Inflammation with an Anti-Inflammatory Diet
Inflammation is a major contributor to fibromyalgia symptoms. Removing inflammatory triggers from the diet can significantly reduce pain and fatigue.
Foods to eliminate:
- Processed sugars and refined carbohydrates
- Gluten and grains (wheat, barley, rye)
- Dairy (for those with sensitivities)
- Nightshade vegetables (tomatoes, peppers, eggplant, potatoes)
- Artificial additives, preservatives, and seed oils
Foods to include:
- Grass-fed meats and wild-caught fish (rich in omega-3s)
- Leafy greens and cruciferous vegetables (anti-inflammatory nutrients)
- Fermented foods (to support gut health)
- Bone broth and collagen (to repair connective tissues)
3. Restore Gut Health and Eliminate Toxins
Research shows that many fibromyalgia patients suffer from gut imbalances, leaky gut syndrome, and microbiome dysfunction. These issues contribute to inflammation, nutrient malabsorption, and immune dysregulation.
Steps to heal the gut:
- Take probiotics and prebiotics to support beneficial gut bacteria
- Eliminate food sensitivities through an elimination diet
- Use digestive enzymes to improve nutrient absorption
- Incorporate detoxification practices such as sauna therapy and dry brushing
4. Optimize Mitochondrial Function for Energy Production
Mitochondria are the energy-producing structures in cells. When they are damaged, fatigue, brain fog, and muscle weakness occur—common symptoms of fibromyalgia.
Ways to boost mitochondrial function:
- CoQ10 and PQQ supplements to enhance energy production
- Magnesium and B vitamins to support ATP (energy) generation
- Intermittent fasting or ketogenic diet to promote cellular repair
- Cold therapy and red light therapy to stimulate mitochondrial function
5. Balance Hormones and Adrenal Function
Fibromyalgia is often linked to hormonal imbalances such as low cortisol, estrogen dominance, or thyroid dysfunction. Optimizing hormone levels can improve sleep, pain tolerance, and emotional stability.
Steps to restore hormonal balance:
- Test for thyroid and adrenal function (TSH, Free T3, Free T4, cortisol levels)
- Adaptogenic herbs (ashwagandha, rhodiola, maca) to support adrenal glands
- Prioritize deep sleep (melatonin, magnesium, and relaxation techniques)
- Reduce stress to lower excess cortisol and prevent adrenal burnout
6. Engage in Gentle Movement and Myofascial Release
Exercise is challenging for fibromyalgia patients, but movement is essential for reducing stiffness, improving circulation, and rebalancing the nervous system.
Recommended movement therapies:
- Slow, low-impact activities (walking, swimming, stretching)
- Myofascial release and trigger point therapy to reduce muscle tension
- Postural realignment exercises to correct imbalances
- Rebounding or vibration therapy to improve lymphatic drainage
7. Improve Sleep Quality for Cellular Repair
Poor sleep worsens fibromyalgia symptoms, making it harder to heal. Prioritizing restorative sleep is a critical part of the protocol.
Sleep optimization strategies:
- Keep a consistent sleep schedule (same bedtime and wake-up time)
- Create a dark, cool sleep environment (avoid blue light and electronic devices)
- Use calming supplements (magnesium glycinate, L-theanine, valerian root)
- Try cognitive behavioral therapy for insomnia (CBT-I) if sleep disturbances persist
How Long Does the Fibromyalgia Reversal Protocol Take?
Healing from fibromyalgia is a gradual process, and results vary from person to person. Some individuals notice improvements within a few weeks, while others may need several months to a year to see significant relief.
Typical timeline for improvement:
- First 4-6 weeks: Reduced bloating, better sleep, slight energy improvements
- 3 months: Noticeable reduction in pain, fewer flare-ups, improved digestion
- 6 months: Increased mobility, less fatigue, more stable mood
- 1 year: Significant symptom reduction, improved overall quality of life
Frequently Asked Questions About the Fibromyalgia Reversal Protocol
1. Can fibromyalgia really be reversed?
While fibromyalgia is considered a chronic condition, many people experience significant symptom reduction and even complete remission by addressing underlying root causes.
2. Do I need to take medications while following this protocol?
Many people reduce their reliance on pain medications and antidepressants as their symptoms improve, but any changes should be made under medical supervision.
3. Is the protocol difficult to follow?
The protocol requires lifestyle changes, but many people find that as their pain and fatigue decrease, it becomes easier to maintain.
4. Can diet alone reverse fibromyalgia?
While diet plays a major role, full recovery often requires nervous system regulation, detoxification, and hormone balance as well.
5. Will this protocol work for everyone with fibromyalgia?
Results vary, but most people experience some level of symptom improvement, especially if they have gut issues, nervous system dysfunction, or mitochondrial problems.
Conclusion: Taking Control of Fibromyalgia and Reclaiming Your Life
The Fibromyalgia Reversal Protocol is a comprehensive approach that focuses on healing the root causes of pain, fatigue, and inflammation. By making targeted changes in diet, movement, nervous system regulation, and sleep, many people find lasting relief from fibromyalgia symptoms.
While healing takes time, this protocol offers a science-backed roadmap to recovery, empowering individuals to take control of their health and rediscover a life free from chronic pain.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores