By: Dr Alex Robber
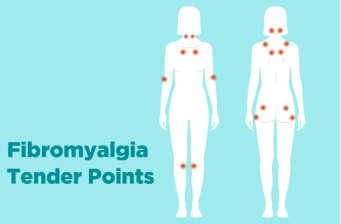
Fibromyalgia impacts 1 in 50 persons, up to 6 million in total. Although only an estimate. It is defined by the symptoms of chronic muscular-skeletal pain with brain fog, behavioral impairment, anxiety, tiredness and sleep disturbances throughout the body. The root cause of fibromyalgia continues uncertain and standard medicine now uses pain relievers and antidepressants to address its symptoms.
Functional medicine, on the other side, seeks to identify the root cause of fibromyalgia and thus treat the underlying problem. The problems below are the top 10 roots of fibromyalgia, according to one Functional Medicine Physician.
Fibromyalgia 10 Root Causes
1. Intolerance of Gluten
Gluten is often described by more than 55 illnesses as the “large masker.” Its symptoms are seldom expressed as digestive but instead as neurological problems, such as sleep disorders, tiredness, anxiety, comport mental problems, cognitive deficiency and pain.
2. Overcrowding Candida
Candida is a yeast genus that thrives in the intestines in a tiny quantity. The problem arises when the wall of the intestines is overgrown and broken down. It thus penetrates the bloodstream and releases toxic matter into the system and creates symptoms such as pain, tiredness and brain fog. Candida was usually overgrown in most patients with fibromyalgia.
3. Toxicity of Mercury
Mercury is an extremely toxic cause of fibromyalgia in our bodies and other chronic diseases such as neurological disorders and autoimmune conditions. The chronic fatigue syndrome is regarded as the potential source of this disease. For this reason, many physicians recommend that their patients seek out a biological dentist and remove their fillings for mercury amalgam.
4. Thyroid
Most individuals with thyroid-related problems do not know it and hypothyroidism affects up to 90 percent. The doctor needs to verify six distinct blood markers to assess the function of the thyroid gland. The doctor must concentrate on the optimal range in place of the standard reference range to evaluate and diagnose thyroid illnesses. The ideal level of the thyroid generates tiredness, sleep disorders, depression and fog for the brain.
Click Here to Visit the Store and find Much More….
5. Fatigue of Adrenal
The principal cause of adrenal tiredness is chronic stress, whether genuine or not. Chronic pain stresses the surrenal glands, although this is not the first surrenal stress in most instances. The most common adrenal stressors are vitamin shortcomings, candida, food intolerances, and mercury toxicity and adrenals should be supported by adapt-genic herbs until the root cause and method of correction have been found.
6. Deficiency of Nutrient
Magnesium, vitamin D and vitamin B12 are usually deficient in fibromyalgia patients. Interestingly, many physicians argue that the increase in magnesium level has helped reverse the situation of the patient. Measuring the red blood cell magnesium level that can be tested in any workshop is the best method of measuring your magnesium level.
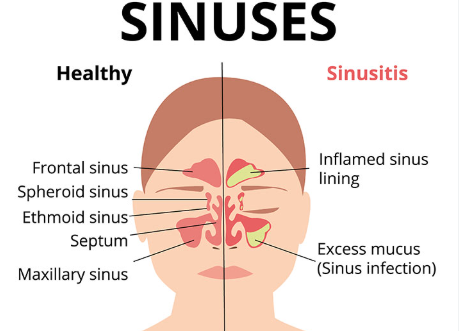
7. Bacterial overgrowth of small intestines (SIBO) and leaky Gut
Were you aware that human cells in the body are larger than bacteria? Use antibiotics and a sugar-rich diet to break the equilibrium, so that nutrients, particularly vitamin B12, can be digested and absorbed. Anybody who is diagnosed with fibromyalgia or a comparable chronic illness should first solve the gut, as this is a vicious cycle with a strong connection between everything.
8. Mycotoxins
The toxic compounds of mycotoxins are toxic molds. The gene that makes one vulnerable to the harmful consequences of mycotoxins is estimated in approximately 25 percent of the population. Unfortunately, standard mold tests do not test for mycotoxins but only for concentrations of molds.
9. Deficiency of Glutathione
Glutathione is a significant antioxidant that plays an significant part in the process of body detoxification. It is recycled into the body, provided it does not exceed normal quantities of toxic matter or the body lacks the required enzymes for glutathione production and recycling. Glutathione or precursors such as mill thistle and NAC has been discovered to help treat fatigue.
10. MTHFR Mutations
A significant metabolic process, MTHFR is an enzyme needed to be methylated. Folate and folic acid are transformed into active forms during this phase so that the body can use them. The body is less likely to methylate and detoxify toxins like lead and mercury through any mutation of the MTHFR. The more mutations one has in the gene, so that the detoxification process remains operative, the higher the needs for folic acid and for methyl B6 and methyl-B12. Stay Healthizes!

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores