Diagnosing fibromyalgia can be a challenging process because it often mimics other conditions such as autoimmune diseases. One diagnostic tool commonly discussed in this context is the Rheumatoid Factor (RF) test. While the RF test is primarily used to diagnose rheumatoid arthritis (RA), it plays a crucial role in ruling out inflammatory autoimmune diseases when evaluating symptoms consistent with fibromyalgia.
This article explores the role of the RF test, its purpose, and how it fits into the broader diagnostic process for fibromyalgia.
What Is the Rheumatoid Factor Test?
The Rheumatoid Factor (RF) test is a blood test that measures the levels of rheumatoid factor—an antibody produced by the immune system that mistakenly attacks the body’s own tissues. Elevated levels of RF are often associated with autoimmune diseases, particularly rheumatoid arthritis (RA).
Purpose of the RF Test:
- Diagnose Rheumatoid Arthritis (RA): High levels of RF are commonly found in individuals with RA, making this test a key diagnostic tool.
- Identify Other Autoimmune Conditions: Elevated RF levels may also be associated with other conditions such as lupus, Sjögren’s syndrome, and certain infections.
- Rule Out Autoimmune Causes: In the context of fibromyalgia, the RF test helps rule out autoimmune diseases as the source of symptoms.
Why Is the RF Test Used in Fibromyalgia Evaluation?
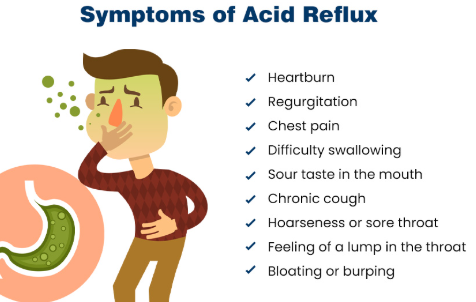
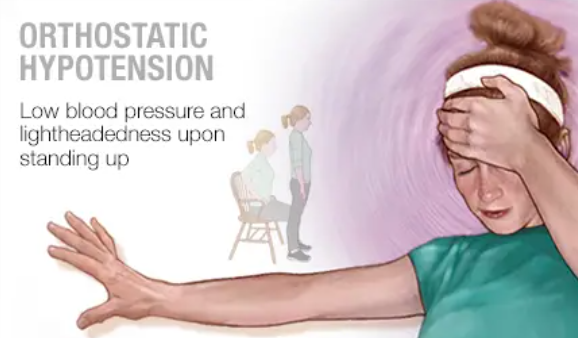
Fibromyalgia is a chronic pain disorder characterized by widespread musculoskeletal pain, fatigue, and other symptoms. However, these symptoms overlap significantly with autoimmune conditions such as RA, making it important to differentiate between the two.
- Ruling Out RA: The RF test is used to determine whether symptoms such as joint pain, stiffness, and swelling are due to RA or fibromyalgia.
- Non-Inflammatory Nature of Fibromyalgia: Unlike RA, fibromyalgia is not associated with inflammation or elevated RF levels. A normal RF result supports a diagnosis of fibromyalgia when other autoimmune conditions are excluded.
How Is the RF Test Performed?
The RF test is a straightforward blood test conducted in a laboratory setting:
- Blood Sample Collection: A small amount of blood is drawn from a vein in the arm.
- Laboratory Analysis: The blood sample is analyzed for the presence and levels of rheumatoid factor antibodies.
- Results Interpretation: The results are measured in units per milliliter (U/mL). High levels of RF are indicative of RA or other autoimmune diseases.
Understanding RF Test Results
1. Negative RF Test Result
A negative RF test result indicates low or undetectable levels of rheumatoid factor in the blood. This result is generally consistent with:
- Fibromyalgia Diagnosis: Since fibromyalgia is not an autoimmune or inflammatory condition, RF levels are typically normal or negative.
- Exclusion of RA: A negative RF result, combined with other diagnostic markers, helps rule out RA as the source of symptoms.
2. Positive RF Test Result
A positive RF test result indicates elevated levels of rheumatoid factor in the blood. This result suggests the presence of an autoimmune condition, most commonly RA.
- Implications for Fibromyalgia Diagnosis: A positive RF test does not confirm fibromyalgia. Instead, it points to autoimmune diseases, requiring further investigation and potentially ruling out fibromyalgia as the sole diagnosis.
Limitations of the RF Test in Fibromyalgia Diagnosis
While the RF test is valuable in differentiating between autoimmune diseases and fibromyalgia, it has limitations:
- Not Specific to Fibromyalgia: The RF test does not provide direct information about fibromyalgia itself, as the condition does not involve elevated RF levels.
- False Positives: Some individuals without RA or autoimmune diseases may have elevated RF levels, complicating the diagnostic process.
- Overlap of Symptoms: Joint pain, stiffness, and fatigue can occur in both fibromyalgia and RA, necessitating additional tests and clinical evaluations.
Complementary Tests for Fibromyalgia Diagnosis
Since fibromyalgia is a diagnosis of exclusion, healthcare providers use multiple tests and evaluations alongside the RF test to rule out other conditions:
- Erythrocyte Sedimentation Rate (ESR): Measures inflammation in the body.
- C-Reactive Protein (CRP) Test: Detects inflammatory markers.
- Antinuclear Antibody (ANA) Test: Screens for autoimmune diseases like lupus.
- Thyroid Function Tests: Rules out hypothyroidism, which shares symptoms with fibromyalgia.
- Vitamin D Levels: Low levels can contribute to musculoskeletal pain.
In addition to these tests, doctors perform a physical exam and assess symptom patterns to confirm a fibromyalgia diagnosis.
Differences Between Fibromyalgia and Rheumatoid Arthritis
The RF test is particularly important in distinguishing fibromyalgia from RA. Understanding the key differences between the two conditions highlights why this test is valuable:
| Feature | Fibromyalgia | Rheumatoid Arthritis (RA) |
|---|---|---|
| Cause | Centralized pain sensitivity | Autoimmune inflammation |
| Inflammation | Not present | Present |
| RF Test Result | Negative | Typically positive |
| Primary Symptoms | Widespread pain, fatigue, sleep issues | Joint pain, swelling, morning stiffness |
| Treatment Approach | Pain management, exercise, CBT | Anti-inflammatory drugs, DMARDs |
How Does the RF Test Fit into the Diagnostic Process?
The RF test is a vital step in the differential diagnosis of fibromyalgia. Since fibromyalgia has no definitive test or biomarker, ruling out other conditions with similar symptoms is essential. The RF test helps doctors determine whether joint pain and stiffness are due to inflammation (as seen in RA) or central pain processing abnormalities (as seen in fibromyalgia).
Conclusion
The Rheumatoid Factor (RF) test plays a key role in distinguishing fibromyalgia from autoimmune diseases such as rheumatoid arthritis. While the RF test does not directly diagnose fibromyalgia, it provides essential information to rule out inflammatory conditions and focus on managing fibromyalgia symptoms effectively.
By understanding the role of the RF test in the diagnostic process, patients can better navigate their healthcare journey, ensuring they receive the right diagnosis and treatment plan. If you are experiencing chronic pain and fatigue, consult with a healthcare provider to discuss the appropriate tests and evaluations for your condition.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores