Introduction
Fibromyalgia is a chronic pain disorder characterized by widespread pain, fatigue, cognitive dysfunction, and sleep disturbances. Diagnosing fibromyalgia has long been challenging due to the lack of definitive laboratory tests or imaging scans. To improve diagnostic accuracy, medical experts have developed fibromyalgia score calculators, which help evaluate symptom severity and determine whether a person meets the criteria for fibromyalgia.
A fibromyalgia score calculator is a tool used by healthcare professionals to measure pain distribution, symptom severity, and overall impact on daily life. It helps standardize the diagnostic process and guide treatment strategies.
This article explores how the fibromyalgia score calculator works, what factors it assesses, and how it benefits both patients and healthcare providers.
What Is a Fibromyalgia Score Calculator?
A fibromyalgia score calculator is a tool designed to assess the presence and severity of fibromyalgia symptoms. It provides a numerical score based on pain locations, symptom intensity, and overall health impact.
This scoring system helps clinicians determine whether a patient meets the diagnostic criteria for fibromyalgia and track symptom progression over time.
How the Fibromyalgia Score Calculator Works
The fibromyalgia score calculator is based on two key components:
- The Widespread Pain Index (WPI) – Measures the number of body regions affected by pain.
- The Symptom Severity Scale (SSS) – Evaluates fatigue, cognitive issues, and other symptoms.
The combined score helps distinguish fibromyalgia from other conditions with similar symptoms.
Key Components of the Fibromyalgia Score
1. Widespread Pain Index (WPI)
The WPI measures pain across 19 specific areas of the body, including:
- Upper body (shoulders, arms, chest)
- Lower body (hips, legs, lower back)
- Axial regions (neck, spine, abdomen)
Each painful area adds one point to the total WPI score.
2. Symptom Severity Scale (SSS)
The SSS evaluates the severity of common fibromyalgia symptoms, such as:
- Fatigue
- Cognitive difficulties (“fibro fog“)
- Waking unrefreshed
- Additional symptoms like headaches, dizziness, and gastrointestinal issues
Each symptom is rated on a scale from 0 to 3, with higher scores indicating greater severity.
Widespread Pain Index (WPI): Measuring Pain Distribution
The WPI component of the fibromyalgia score calculator requires patients to identify the regions where they experience persistent pain.
A score is calculated by counting the number of painful areas out of the 19 designated regions.
- Mild cases may have a WPI score between 3 and 7.
- Severe cases may have a WPI score above 12.
The higher the WPI score, the more widespread the pain is across the body.
Symptom Severity Scale (SSS): Evaluating Additional Symptoms
The SSS evaluates the impact of non-pain symptoms associated with fibromyalgia.
Each of the three primary symptoms—fatigue, cognitive difficulties, and sleep disturbances—is scored from 0 (none) to 3 (severe).
Additional symptoms such as irritable bowel syndrome (IBS), headaches, and sensitivity to noise or light are also factored into the SSS score.
- A low SSS score (0-5) suggests milder symptoms.
- A high SSS score (9-12) indicates severe symptom burden.
How the Total Fibromyalgia Score Is Calculated
The total fibromyalgia score is the sum of the WPI and SSS scores.
- Fibromyalgia is diagnosed if a patient meets either of the following criteria:
- WPI of 7 or more and SSS of 5 or more.
- WPI between 3 and 6, with an SSS of 9 or more.
This calculation helps doctors make a consistent and evidence-based diagnosis.
Interpreting Your Fibromyalgia Score
The final score provides an indication of symptom severity:
- Mild fibromyalgia (Total score: 6-10) – Symptoms are manageable with lifestyle changes.
- Moderate fibromyalgia (Total score: 11-15) – Symptoms significantly impact daily life.
- Severe fibromyalgia (Total score: 16+) – Requires intensive treatment and symptom management.
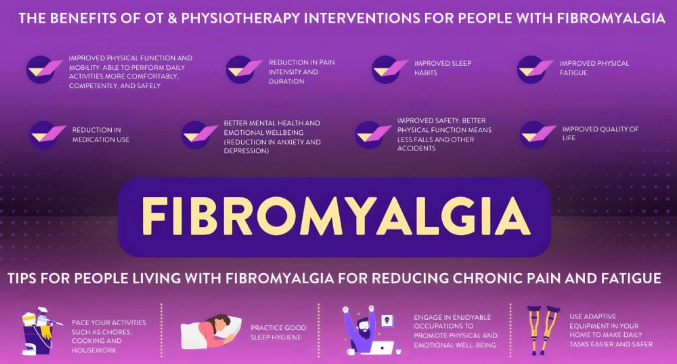
Why a Fibromyalgia Score Calculator Is Useful
- Improves diagnostic accuracy by standardizing symptom evaluation.
- Helps track symptom progression over time.
- Guides treatment decisions, including medication and therapy options.
- Validates patient experiences, making it easier to communicate symptoms to healthcare providers.
Limitations of Fibromyalgia Score Calculators
- Cannot replace a clinical diagnosis – Must be used alongside medical evaluation.
- Does not measure emotional and social impact of fibromyalgia.
- Variability in symptom perception can affect scoring accuracy.
Using the Fibromyalgia Score to Guide Treatment
- Low scores may require lifestyle adjustments like exercise and stress management.
- Moderate scores may benefit from medications, physical therapy, and cognitive behavioral therapy.
- High scores may require a multidisciplinary approach, combining medication, pain management, and lifestyle interventions.
The Future of Fibromyalgia Diagnosis and Scoring Systems
Research is exploring biomarker–based tests and AI-powered diagnostic tools to improve accuracy. Future advancements may lead to:
- More personalized treatment plans.
- Objective tests to confirm fibromyalgia.
- Better symptom-tracking apps for patients.
Conclusion
The fibromyalgia score calculator is a valuable tool for assessing symptom severity, guiding diagnosis, and tracking progress over time. While it does not replace medical evaluation, it helps standardize the diagnostic process and provides a structured way to understand the condition’s impact.
As research continues, improved scoring systems and diagnostic tools will enhance fibromyalgia care, ensuring earlier diagnosis and better treatment options for millions of patients worldwide.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores