Introduction
Fibromyalgia is a chronic condition that affects multiple body systems, causing widespread pain, fatigue, cognitive difficulties, and sensory disturbances. One lesser-known but frustrating symptom is speech problems.
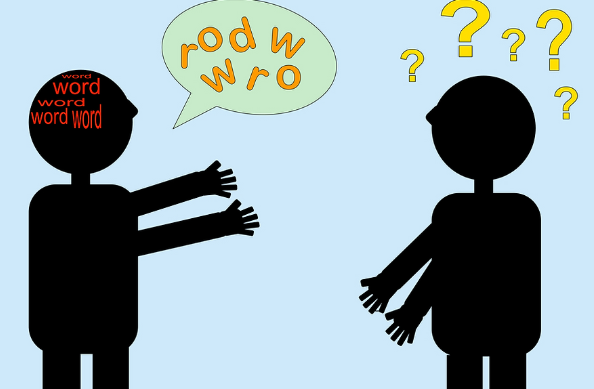
Many individuals with fibromyalgia report difficulties with word recall, slurred speech, difficulty articulating words, and slow speech processing. These speech disturbances can make communication challenging and lead to frustration in daily interactions.
Understanding the connection between fibromyalgia and speech problems can help individuals manage symptoms, reduce anxiety, and seek appropriate coping strategies.
1. How Does Fibromyalgia Cause Speech Problems?
Speech problems in fibromyalgia are primarily related to cognitive dysfunction, also known as “fibro fog.” The nervous system dysfunction in fibromyalgia affects how the brain processes and articulates words.
Speech difficulties may be caused by:
✔ Cognitive impairment (“fibro fog”) – Difficulty recalling words or forming coherent sentences.
✔ Neurological dysfunction – Slowed speech processing and trouble organizing thoughts.
✔ Fatigue and exhaustion – Lack of energy to articulate words clearly.
✔ Muscle tension or pain – Stiffness in the jaw or throat affecting pronunciation.
✔ Sensory overload – Difficulty focusing on speech due to external distractions.
2. Common Speech Problems in Fibromyalgia
Speech issues can manifest in different ways for fibromyalgia patients. Some of the most common speech-related symptoms include:
2.1 Word-Finding Difficulties (Aphasia-like Symptoms)
✔ Many people with fibromyalgia experience word retrieval issues, struggling to find the right words during conversations.
✔ Speech may include long pauses, stuttering, or substituting incorrect words.
✔ This issue can worsen with stress, fatigue, or sensory overload.
2.2 Slurred or Slow Speech
✔ Fibromyalgia can cause neuromuscular fatigue, making it difficult to control the muscles used for speaking.
✔ Speech may sound slurred, slow, or mumbled, especially during flare-ups or after exertion.
✔ Some individuals may experience difficulty pronouncing complex words.
2.3 Trouble Organizing Thoughts While Speaking
✔ Cognitive dysfunction in fibromyalgia can lead to difficulty structuring sentences.
✔ Some individuals may start speaking but forget the point of their conversation mid-sentence.
✔ This can cause frustration, social anxiety, and embarrassment.
2.4 Difficulty Understanding or Processing Language
✔ Some fibromyalgia patients have trouble understanding spoken words, especially when distracted.
✔ Background noise or sensory overload can worsen speech comprehension.
✔ Processing delays can make it hard to respond quickly in conversations.
2.5 Hoarseness or Vocal Fatigue
✔ Fibromyalgia-related fatigue can cause the voice to become hoarse, weak, or strained.
✔ Speaking for long periods can lead to vocal exhaustion or discomfort.
✔ Dry mouth, a common symptom in fibromyalgia, may also contribute to voice strain.
3. Causes of Speech Problems in Fibromyalgia
Several factors contribute to speech difficulties in fibromyalgia. Understanding these causes can help individuals manage their symptoms more effectively.
3.1 Fibro Fog and Cognitive Dysfunction
✔ Fibro fog affects memory, concentration, and verbal fluency.
✔ The brain struggles with word recall, processing speed, and organizing speech.
✔ Mental fatigue makes it difficult to keep up with conversations.
3.2 Neurological Dysfunction
✔ Fibromyalgia is linked to abnormal nervous system responses.
✔ Disruptions in nerve signaling may contribute to slowed speech processing and difficulty articulating words.
✔ Some individuals report feeling like their brain and mouth are “disconnected“.
3.3 Fatigue and Physical Exhaustion
✔ Chronic fatigue makes verbal communication more effortful.
✔ Extreme exhaustion can lead to slurred or slowed speech.
✔ Some individuals feel mentally drained after long conversations.
3.4 Muscle Tension and Pain
✔ Fibromyalgia causes widespread muscle pain and tension, including in the jaw, neck, and throat.
✔ Jaw stiffness (TMJ dysfunction) can make speaking uncomfortable.
✔ Pain in the throat muscles can lead to strained or hoarse speech.
3.5 Anxiety and Stress
✔ Fibromyalgia is often associated with anxiety and social stress, which can exacerbate speech difficulties.
✔ Nervousness may cause stuttering, mind blanks, or difficulty articulating thoughts.
✔ High stress levels can lead to increased fibro fog and slowed speech processing.
4. How Speech Problems Impact Daily Life
4.1 Communication Struggles
✔ Difficulty finding words or speaking clearly can lead to frustration.
✔ Social interactions may become stressful or exhausting.
✔ Some individuals may feel embarrassed or self-conscious about their speech difficulties.
4.2 Work and Professional Challenges
✔ Trouble communicating clearly can make meetings and presentations difficult.
✔ Slow speech processing may lead to delayed responses in conversations.
✔ Workplace stress can worsen cognitive and speech-related symptoms.
4.3 Social and Emotional Impact
✔ Speech problems may cause avoidance of social situations.
✔ Some individuals experience depression or isolation due to communication struggles.
✔ Feeling misunderstood can increase frustration and self-doubt.
5. Tips for Managing Speech Problems in Fibromyalgia
Although speech difficulties can be frustrating, several strategies can help improve verbal communication and reduce anxiety.
5.1 Slow Down and Take Your Time
✔ Speak slowly and pause when needed to gather your thoughts.
✔ If struggling with word recall, use simpler words or descriptions.
✔ Don’t be afraid to ask for patience from others.
5.2 Stay Hydrated and Rest Your Voice
✔ Drink plenty of water to prevent dry mouth and vocal strain.
✔ Take breaks from speaking when feeling fatigued or hoarse.
5.3 Reduce Background Noise and Distractions
✔ Have conversations in quiet environments to improve focus.
✔ Minimize distractions to help with speech processing.
5.4 Use Writing or Assistive Communication Tools
✔ Keep a notepad or phone notes handy to jot down thoughts.
✔ Use speech-to-text apps when struggling with verbal communication.
5.5 Practice Speech and Cognitive Exercises
✔ Try word-recall games or puzzles to improve verbal fluency.
✔ Reading aloud can help strengthen speech coordination and processing speed.
5.6 Manage Stress and Anxiety
✔ Use deep breathing techniques to reduce nervousness while speaking.
✔ Engage in mindfulness or relaxation exercises to ease mental tension.
✔ Talk to a therapist if anxiety is worsening speech problems.
6. When to Seek Medical Help
Although speech difficulties are common in fibromyalgia, it’s important to seek medical attention if:
✔ Speech problems are severe, persistent, or getting worse.
✔ There are sudden or unexplained speech changes, such as slurred speech or difficulty forming sentences.
✔ You experience difficulty swallowing, drooping facial muscles, or other neurological symptoms.
A doctor may conduct neurological exams, speech therapy assessments, or cognitive evaluations to determine if other conditions are contributing to speech problems.
7. Conclusion: Managing Speech Difficulties in Fibromyalgia
Speech problems in fibromyalgia can be frustrating and challenging, but understanding their causes can help individuals develop coping strategies and communication techniques.
By managing fibro fog, reducing stress, improving hydration, and practicing speech exercises, individuals can enhance verbal communication and reduce frustration.
If speech issues become severe, seeking medical guidance can provide additional support and treatment options.
Would you like recommendations for cognitive exercises or speech therapy techniques for fibromyalgia?

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores