Fibromyalgia is a chronic condition that primarily causes widespread pain, fatigue, and cognitive dysfunction, but it is also associated with a range of other symptoms, many of which can significantly impact a person’s daily life. One such symptom is acid reflux, a condition that is commonly characterized by the backward flow of stomach acid into the esophagus. Individuals with fibromyalgia often experience acid reflux as a secondary symptom, complicating their condition and requiring specific management strategies. In this article, we will explore the relationship between fibromyalgia and acid reflux, the symptoms to look out for, and how individuals can effectively manage this issue.
What is Fibromyalgia?
Fibromyalgia is a chronic disorder that is primarily marked by widespread musculoskeletal pain, fatigue, disrupted sleep, and cognitive difficulties. While the exact cause of fibromyalgia remains unknown, it is believed to be linked to abnormalities in how the brain processes pain signals, leading to an increased sensitivity to pain. Along with these hallmark symptoms, fibromyalgia can also cause a variety of other issues, including digestive problems such as acid reflux, gastrointestinal distress, and irritable bowel syndrome (IBS). These co-occurring symptoms can further complicate the daily challenges faced by those living with fibromyalgia.
Understanding Acid Reflux
Acid reflux occurs when stomach acid or bile from the stomach flows backward into the esophagus, the tube that connects the mouth to the stomach. This backward flow can lead to discomfort, irritation, and a variety of symptoms. Acid reflux is also known as gastroesophageal reflux disease (GERD) when it occurs frequently and causes significant disruption to daily life. Common symptoms of acid reflux include heartburn, regurgitation of food or acid, chest pain, and difficulty swallowing.
While acid reflux is common in the general population, individuals with fibromyalgia appear to be at an increased risk of experiencing this condition, likely due to the complex interplay between fibromyalgia, the gastrointestinal system, and the central nervous system.
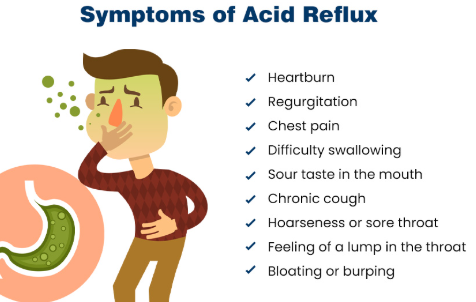
Common Symptoms of Acid Reflux in Fibromyalgia
Acid reflux symptoms can vary in severity and frequency, but individuals with fibromyalgia may experience the following symptoms:
1. Heartburn and Chest Pain
Heartburn is the hallmark symptom of acid reflux, characterized by a burning sensation in the chest, often after eating or when lying down. This sensation occurs when stomach acid irritates the esophagus. People with fibromyalgia may experience this discomfort more frequently, as the body’s heightened sensitivity to pain can amplify the sensation of heartburn. In some cases, individuals may also experience chest pain that mimics the feeling of a heart attack, which can be alarming and lead to unnecessary worry.
2. Regurgitation
Regurgitation is the sensation of food or acidic fluid rising into the mouth or throat. This can occur alongside heartburn and may cause an unpleasant sour or bitter taste in the mouth. People with fibromyalgia who experience regurgitation may find that it is triggered by certain foods or even by lying down after eating.
3. Difficulty Swallowing (Dysphagia)
Some individuals with acid reflux in fibromyalgia may experience difficulty swallowing, known as dysphagia. This sensation occurs when food or liquid feels as though it is stuck in the throat or chest. The discomfort can range from mild to severe, and in some cases, it may be associated with the irritation caused by stomach acid in the esophagus.
4. Chronic Cough or Throat Clearing
Acid reflux can lead to a chronic cough or frequent throat clearing, as the acid irritates the throat and airways. People with fibromyalgia may be more sensitive to this irritation, and the constant need to clear the throat can be disruptive and uncomfortable. In some cases, acid reflux-related coughing may worsen at night or during sleep.
5. Hoarseness or Sore Throat
Acid reflux can also cause a sore throat or hoarseness, as stomach acid irritates the vocal cords and throat. This can be particularly problematic for individuals with fibromyalgia who may already experience throat discomfort as part of their condition. Chronic sore throat and hoarseness can interfere with daily activities, including speaking and eating.
6. Nausea
Nausea is a common symptom of both fibromyalgia and acid reflux. When acid reflux occurs, it can cause an upset stomach and feelings of nausea, particularly after eating. The overlap of these symptoms can make it difficult to determine whether nausea is caused by fibromyalgia, acid reflux, or a combination of both.
Causes of Acid Reflux in Fibromyalgia
The exact cause of acid reflux in fibromyalgia remains unclear, but several factors may contribute to the increased prevalence of this condition in individuals with fibromyalgia. These factors include:
1. Gastrointestinal Dysregulation
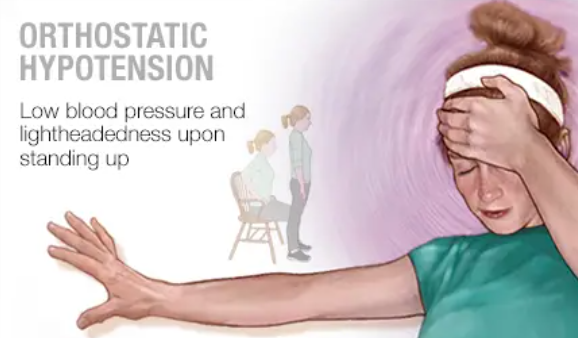
Individuals with fibromyalgia often experience dysfunction in the gastrointestinal (GI) system, which can contribute to acid reflux. The autonomic nervous system (ANS), which controls involuntary bodily functions such as digestion, is often dysregulated in fibromyalgia, leading to slower gastric emptying, increased acid production, and heightened sensitivity to stomach discomfort. These disturbances in the digestive process may increase the likelihood of acid reflux symptoms.
2. Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome (IBS) is a common gastrointestinal disorder that frequently coexists with fibromyalgia. IBS can cause a variety of symptoms, including bloating, abdominal pain, constipation, and diarrhea. IBS may also contribute to the development of acid reflux, as the digestive system becomes more sensitive and prone to irregularities. Individuals with both IBS and fibromyalgia may experience a greater intensity of gastrointestinal distress, including acid reflux symptoms.
3. Medication Side Effects
Certain medications used to treat fibromyalgia symptoms, such as muscle relaxants, pain relievers, and antidepressants, can contribute to acid reflux. For example, nonsteroidal anti-inflammatory drugs (NSAIDs), commonly used for pain management, can irritate the stomach lining and exacerbate acid reflux symptoms. Additionally, medications that affect the central nervous system, including some antidepressants and anti-anxiety drugs, may alter the functioning of the lower esophageal sphincter (LES), leading to increased acid reflux.
4. Stress and Anxiety
Stress and anxiety are common in individuals with fibromyalgia due to chronic pain and fatigue, and these emotional states can contribute to gastrointestinal distress, including acid reflux. The stress response can lead to increased stomach acid production, relaxation of the LES, and altered digestion, all of which can exacerbate acid reflux symptoms.
5. Sleep Disturbances
Sleep disturbances, such as difficulty falling or staying asleep, are common in fibromyalgia. Poor sleep quality can worsen acid reflux, as lying down during sleep allows stomach acid to flow back into the esophagus more easily. Individuals with fibromyalgia who experience both acid reflux and sleep issues may find that their symptoms are most pronounced at night, interfering with both rest and digestion.
Managing Acid Reflux in Fibromyalgia
While acid reflux can be a challenging symptom to manage in fibromyalgia, there are several strategies that individuals can adopt to reduce symptoms and improve their overall well-being. A combination of lifestyle changes, dietary adjustments, and medical treatments can provide relief.
1. Dietary Modifications
Making changes to the diet can significantly reduce acid reflux symptoms. Avoiding trigger foods, such as spicy dishes, acidic foods (e.g., citrus and tomatoes), chocolate, caffeine, and fatty foods, can help prevent acid reflux flare-ups. Eating smaller, more frequent meals instead of large meals can also reduce pressure on the stomach and decrease the likelihood of acid reflux. Additionally, it is recommended to avoid eating too close to bedtime, as lying down soon after eating increases the risk of acid reflux.
2. Stress Management
Since stress is a major contributor to acid reflux in fibromyalgia, managing stress is crucial for symptom relief. Stress-reduction techniques such as mindfulness meditation, deep breathing exercises, yoga, and cognitive-behavioral therapy (CBT) can help regulate the body’s stress response, reduce anxiety, and alleviate gastrointestinal symptoms, including acid reflux.
3. Medication Adjustments
In some cases, medications such as proton pump inhibitors (PPIs) or H2 blockers may be prescribed to reduce stomach acid production and alleviate acid reflux symptoms. If medications used to treat fibromyalgia are contributing to acid reflux, it may be necessary to consult with a healthcare provider to adjust the treatment regimen. Antacids and other over-the-counter medications may also provide temporary relief from acid reflux symptoms.
4. Elevating the Head While Sleeping
To prevent acid reflux during the night, individuals can try elevating the head of the bed by 6 to 8 inches. This helps prevent stomach acid from flowing back into the esophagus while sleeping. Using a wedge pillow or an adjustable bed may be beneficial for this purpose.
5. Regular Exercise
Although exercise can sometimes be challenging for individuals with fibromyalgia, gentle physical activity, such as walking or swimming, can help improve digestion, reduce stress, and enhance overall well-being. Exercise can also aid in weight management, which may further reduce the risk of acid reflux.
Conclusion
Acid reflux is a common and distressing symptom experienced by many individuals with fibromyalgia. The relationship between fibromyalgia and acid reflux is multifactorial, involving gastrointestinal dysregulation, medication side effects, stress, and sleep disturbances. By understanding the connection between these two conditions and adopting effective management strategies, individuals with fibromyalgia can reduce the impact of acid reflux on their daily lives. With the right combination of lifestyle changes, dietary modifications, stress management, and medical treatments, it is possible to alleviate acid reflux symptoms and improve overall quality of life.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores