What I Mean When I Say I’m Having a Fibro Flare-Up
There’s a moment when the words leave my mouth and I brace myself for the response. I say, “I’m having a fibro flare-up,” and I can already see the confusion in someone’s eyes. Maybe they nod sympathetically. Maybe they change the subject. Or maybe they ask, “What does that mean?”
The phrase is short and simple. But the reality behind it is anything but.
Living with fibromyalgia means navigating a constant undercurrent of pain, fatigue, and sensory overload. When I say I’m having a flare-up, I’m not just describing a bad day. I’m signaling that the already-challenging symptoms have intensified, often without warning, and that my body is no longer cooperating in even the most basic ways.
Here’s what I really mean when I say I’m having a fibro flare-up.
Pain Has Taken Over
On a normal day, I live with pain. It’s background noise—constant but manageable. But during a flare-up, that pain becomes the loudest sound in the room. It’s not just aching joints or sore muscles. It’s burning, stabbing, radiating discomfort that can affect any part of my body without a predictable pattern.
The pain might settle in my shoulders one hour and shoot down my legs the next. Clothes feel too tight, even when they’re loose. Light touches can feel like pressure, and every step is a calculated decision.
This isn’t soreness. It’s a full-body rebellion.
My Brain Feels Foggy and Far Away
One of the lesser-known aspects of fibromyalgia is “fibro fog”—and during a flare, it becomes a thick mental cloud. Words escape me. Thoughts vanish mid-sentence. I might forget what I’m doing in the middle of a task. Simple decisions become impossible puzzles.
When I say I’m having a flare, I mean I’m struggling to think clearly. Conversations take effort. Concentration feels impossible. And that’s not laziness—it’s neurological overload.
Exhaustion That Sleep Doesn’t Fix
Fatigue is a constant companion with fibromyalgia. But during a flare-up, it’s more than just being tired. It’s like someone has drained my energy and replaced it with lead. Getting out of bed feels monumental. Taking a shower becomes a question of whether I can stand long enough.
Even if I’ve slept all night, I wake up unrefreshed. My body aches, my mind is slow, and even breathing deeply feels like effort.
So when I say I’m in a flare, it’s not about being sleepy. It’s a kind of exhaustion that’s hard to describe and harder to push through.
My Skin and Senses Are on Edge
During a flare-up, the world feels louder, brighter, and more irritating. Lights can feel piercing. Sounds that wouldn’t normally bother me suddenly feel overwhelming. My skin can become hypersensitive, reacting to changes in temperature or even soft fabrics.
The sensory overload adds to the feeling of being trapped in my own body. Crowded spaces feel unbearable. Socializing becomes emotionally draining.
So when I say I’m flaring, I mean my senses are screaming, and I need quiet, space, and time to recover.
I’m Not Canceling Plans, I’m Surviving
One of the hardest parts of a fibro flare is its invisibility. I may not look any different. I may smile through a video call or reply to a message. But behind the scenes, I’m struggling to function.
When I cancel plans, it’s not because I’m flaking out. It’s because my body has decided that getting dressed, leaving the house, or even sitting upright is too much. And when I say I’m having a flare, what I’m really saying is: I need to listen to my body, or it will scream louder.
There’s No Quick Fix
People often ask what they can do to help or what I take to make it go away. The truth is, there’s no easy fix. Rest helps. Heat helps. Medications and supplements may take the edge off. But a flare-up has its own timeline.
What I need most is patience, support, and understanding. I don’t need someone to fix me. I need someone to walk with me, even if it’s just in spirit.
I Feel Frustrated and Vulnerable
Every flare-up reminds me that I’m not in control. It forces me to slow down, cancel things I care about, and cope with pain that others can’t see. That loss of control can be emotionally exhausting.
When I say I’m having a flare, I’m also saying I feel vulnerable. I might feel guilty, ashamed, or scared about how long it will last. I may not want to talk about it, but I don’t want to be ignored either.
Frequently Asked Questions
1. What is a fibromyalgia flare-up?
A flare-up is a period when fibromyalgia symptoms—such as pain, fatigue, and brain fog—become significantly worse and harder to manage.
2. How long do flare-ups last?
Flares can last anywhere from a few hours to several days or even weeks. Duration varies widely from person to person.
3. What causes a fibromyalgia flare-up?
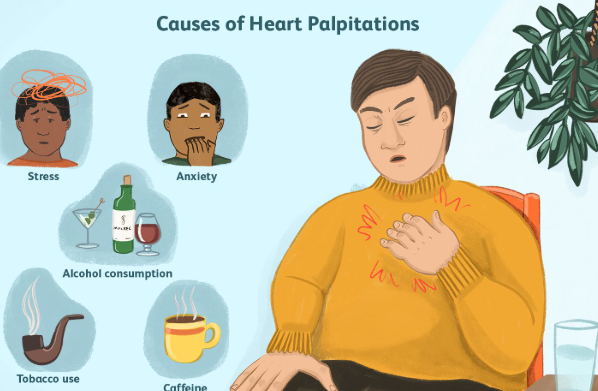
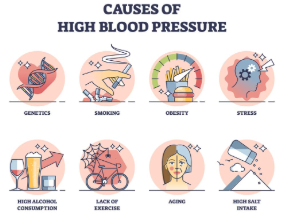
Triggers include stress, overexertion, weather changes, poor sleep, illness, or even diet changes. Sometimes, flares occur without a clear reason.
4. How can I help someone experiencing a flare?
Be patient, offer support without pushing, and respect their need for rest. Small gestures like meals, check-ins, or understanding cancellations mean a lot.
5. Can flare-ups be prevented?
While not always preventable, managing stress, pacing activities, and maintaining a healthy lifestyle can reduce the frequency and severity of flares.
6. Should I go to the doctor during a flare?
If symptoms are unusually severe or if new symptoms appear, it’s wise to consult a healthcare provider to rule out other conditions.
So when I say I’m having a fibro flare-up, I’m not just being dramatic. I’m sharing something real, something that disrupts every part of my day. I’m asking for space, for understanding, and sometimes for help.
Behind that one sentence lies a world of pain, fatigue, and quiet strength. And more than anything, I want people to understand what those words really mean—not just hear them, but feel the truth within them.
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores