Fibromyalgia is a complex chronic pain disorder that affects millions of people worldwide. It is characterized by widespread musculoskeletal pain, fatigue, cognitive dysfunction, and sleep disturbances. While its exact cause remains unknown, researchers have explored various factors, including genetics, environmental triggers, and neurological dysfunction.
One of the most debated questions in fibromyalgia research is: Is fibromyalgia genetic? Many patients report a family history of the condition, suggesting a hereditary component. However, genetics alone may not fully explain why some people develop fibromyalgia while others do not.
This article explores the relationship between fibromyalgia and genetics, examining whether the disorder is inherited, the role of specific genes, and how genetic predisposition interacts with environmental factors.
What is Fibromyalgia?
Fibromyalgia is a neurological disorder that affects the way the brain and nervous system process pain signals. Instead of being caused by joint damage or inflammation, fibromyalgia pain results from an overactive pain response in the central nervous system.
Common Symptoms of Fibromyalgia
- Widespread musculoskeletal pain lasting for more than three months
- Fatigue and sleep disturbances (non-restorative sleep)
- Brain fog (difficulty concentrating and memory issues)
- Increased sensitivity to pain, temperature, and pressure
- Digestive issues, including irritable bowel syndrome (IBS)
- Numbness or tingling in hands and feet
Despite the high prevalence of fibromyalgia, its exact cause remains unknown. While stress, infections, and physical trauma can trigger symptoms, researchers believe genetic factors also play a significant role.
Is Fibromyalgia Genetic?
While fibromyalgia is not considered a purely genetic disorder, research suggests that genetic factors contribute to its development. Studies show that first-degree relatives (parents, siblings, and children) of fibromyalgia patients are more likely to develop the condition than those without a family history.
Key Evidence Supporting the Genetic Link
- Family studies indicate that fibromyalgia runs in families, with first-degree relatives being up to eight times more likely to develop the disorder.
- Twin studies have shown that identical twins are more likely to share fibromyalgia symptoms than fraternal twins, suggesting a genetic component.
- Genetic markers linked to pain processing, neurotransmitter function, and stress response have been identified in fibromyalgia patients.
However, genetics alone do not determine whether a person will develop fibromyalgia. Instead, a combination of genetic susceptibility and environmental factors appears to influence its onset.
Genes Associated with Fibromyalgia
Several genes related to pain sensitivity, neurotransmitter regulation, and stress response have been linked to fibromyalgia. Some of the most studied genetic markers include:
1. Serotonin Transporter Gene (5-HTT or SLC6A4)
- This gene affects serotonin levels, which play a crucial role in mood regulation and pain perception.
- Variants of this gene have been linked to increased pain sensitivity and higher fibromyalgia risk.
2. Catechol-O-Methyltransferase (COMT) Gene
- The COMT gene is responsible for breaking down dopamine, a neurotransmitter involved in pain modulation.
- Some variations of the COMT gene have been associated with lower pain tolerance, a common trait in fibromyalgia patients.
3. Dopamine Receptor Genes (DRD4 and DRD3)
- Dopamine helps regulate mood, motivation, and pain processing.
- Certain dopamine receptor gene variations have been linked to chronic pain conditions, including fibromyalgia.
4. Glutamate-Related Genes (GRIA3 and GRIN2A)
- Glutamate is an excitatory neurotransmitter that plays a role in pain signaling.
- Some studies suggest that excess glutamate activity in fibromyalgia patients may contribute to chronic pain and fatigue.
5. HLA Genes (Human Leukocyte Antigen)
- The HLA system is involved in immune function and inflammation.
- Variants of HLA genes have been linked to fibromyalgia and other chronic pain conditions, suggesting a possible autoimmune connection.
Genetics vs. Environmental Triggers: What Causes Fibromyalgia?
Although genetics may increase susceptibility, fibromyalgia does not follow a clear inheritance pattern. Instead, it is believed to be a multifactorial condition, meaning that both genetics and environmental factors play a role.
Common Environmental Triggers for Fibromyalgia
- Physical Trauma – Accidents, injuries, or surgery can trigger fibromyalgia in genetically predisposed individuals.
- Infections – Viral infections (such as Epstein-Barr virus) and bacterial infections have been linked to fibromyalgia onset.
- Chronic Stress – Long-term emotional or psychological stress can disrupt pain processing and contribute to fibromyalgia symptoms.
- Hormonal Changes – Women are more likely to develop fibromyalgia, possibly due to hormonal fluctuations.
- Sleep Disorders – Poor sleep quality can lower pain tolerance and increase fibromyalgia symptoms.
The “Two-Hit Hypothesis”
Some researchers propose a “two-hit hypothesis“, where individuals with a genetic predisposition to fibromyalgia develop the condition only after experiencing a significant environmental trigger (such as trauma, infection, or chronic stress).
How is Fibromyalgia Diagnosed?
Since fibromyalgia does not have a definitive genetic test, diagnosis is based on:
- A thorough medical history and symptom assessment
- Physical examination to check for tender points and widespread pain
- Ruling out other conditions (such as arthritis, lupus, or thyroid disorders)
Because fibromyalgia symptoms overlap with many other conditions, doctors may use genetic and biomarker research to refine future diagnostic tools.
Can Fibromyalgia Be Inherited?
While fibromyalgia itself is not directly inherited, having a family history of fibromyalgia increases the likelihood of developing the condition. However, genetic predisposition alone is not enough to cause fibromyalgia—environmental and lifestyle factors play a critical role.
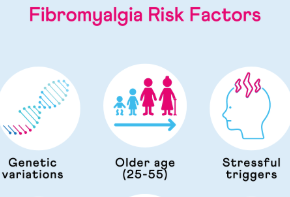
Who is at Higher Risk?
- People with a family history of fibromyalgia or chronic pain conditions
- Women (especially between ages 30-50)
- Individuals who have experienced severe physical or emotional trauma
- Those with co-existing conditions such as IBS, migraines, or depression
Future of Fibromyalgia Research: Can Genetics Lead to a Cure?
The study of fibromyalgia genetics is still evolving, and researchers hope that identifying key genetic markers will lead to:
- More accurate diagnostic tests
- Personalized treatment approaches based on genetic profiles
- Targeted medications that address pain-processing abnormalities
By understanding how genetic predisposition interacts with environmental triggers, scientists aim to develop better prevention and treatment strategies for fibromyalgia in the future.
Final Thoughts: Are Your Genes to Blame for Fibromyalgia?
- Fibromyalgia has a genetic component, but it is not solely inherited like some other diseases.
- Multiple genes related to pain sensitivity and neurotransmitter function may contribute to fibromyalgia risk.
- Environmental factors (stress, trauma, infections) play a crucial role in triggering symptoms.
- A family history of fibromyalgia increases your risk, but lifestyle changes and early management can help reduce symptoms.
If you suspect you have fibromyalgia or have a family history of the condition, consult a healthcare provider for an accurate diagnosis and personalized treatment plan.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores