Introduction
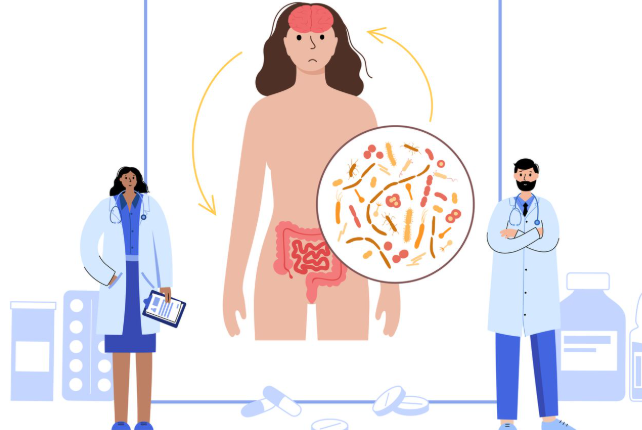
Fibromyalgia is a chronic pain disorder that affects millions of people worldwide, yet it remains widely misunderstood. While medical research has made progress in identifying fibromyalgia as a neurological pain processing disorder, society and cultural attitudes still influence how the condition is perceived, diagnosed, and treated.
Many people with fibromyalgia face skepticism, stigma, and barriers to adequate care, largely due to misconceptions and cultural attitudes toward chronic pain, disability, and invisible illnesses. This article explores the impact of society and culture on fibromyalgia, examining how public perception, workplace challenges, gender biases, and healthcare disparities shape the lives of those with this condition.
The Social Perception of Fibromyalgia
Public perception of fibromyalgia is often shaped by misinformation, stereotypes, and medical uncertainty.
- Some people view fibromyalgia as a “made-up” condition or an excuse for avoiding work.
- Others believe it is just another form of depression or anxiety, rather than a physical disorder.
- The lack of visible symptoms makes it harder for the general public to understand the daily struggles of fibromyalgia patients.
These misconceptions lead to social isolation and frustration for those living with fibromyalgia.
The Stigma of Invisible Illnesses
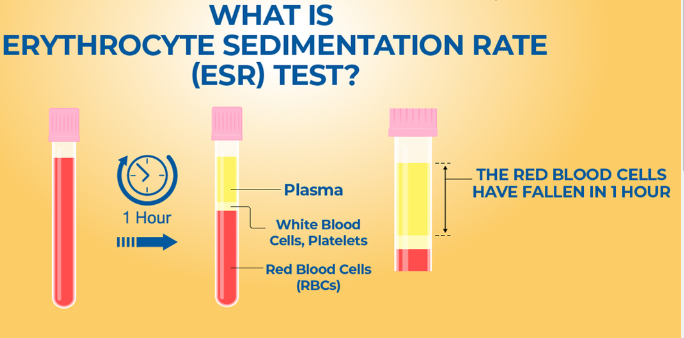
Because fibromyalgia does not have obvious physical signs, it falls into the category of invisible illnesses.
- Unlike conditions such as arthritis or multiple sclerosis, fibromyalgia symptoms are not visible on medical scans or tests.
- Patients often feel pressured to “prove” their pain to family, employers, and even doctors.
- Many experience medical gaslighting, where healthcare providers dismiss their symptoms as psychological or exaggerated.
This stigma creates additional emotional distress and can discourage people from seeking proper care.
How Cultural Attitudes Influence Fibromyalgia Recognition
Different cultures have varying perspectives on chronic pain and disability, affecting how fibromyalgia is diagnosed and treated.
- Western cultures often focus on biological causes of illness, leading to skepticism about conditions with no clear physical markers.
- Some Asian and African cultures view chronic pain as a spiritual imbalance rather than a medical condition.
- In some regions, discussing chronic illness is taboo, preventing open conversations about fibromyalgia.
These cultural differences impact how quickly patients seek medical help and whether they receive a proper diagnosis.
Gender Bias in Fibromyalgia Diagnosis and Treatment
Fibromyalgia disproportionately affects women, leading to gender bias in medical treatment and societal perception.
- Women’s pain is more likely to be dismissed as emotional or stress-related.
- Studies show that female patients wait longer for pain treatment than men.
- Men with fibromyalgia often face even greater challenges, as the condition is stereotyped as a “women’s disease.”
This gender bias leads to delayed diagnoses and inadequate pain management for many fibromyalgia patients.
Fibromyalgia in the Workplace: Challenges and Discrimination
Many fibromyalgia patients face workplace discrimination due to:
- Employers not believing their condition is real.
- Difficulty getting workplace accommodations for chronic pain and fatigue.
- Fear of job loss or reduced hours due to frequent sick days.
Some workers are forced to leave their jobs, while others struggle in silence to avoid stigma or retaliation.
Media Representation of Fibromyalgia: Raising Awareness or Spreading Misinformation?
Media coverage of fibromyalgia is inconsistent, sometimes helping to spread awareness while at other times promoting misconceptions.
- Some news reports and TV shows depict fibromyalgia as an “imaginary” illness.
- Certain celebrities have helped increase awareness, but skeptics question their experiences.
- Misinformation online can lead to false cures and unproven treatments, taking advantage of vulnerable patients.
Accurate media representation is essential to improving public understanding of fibromyalgia.
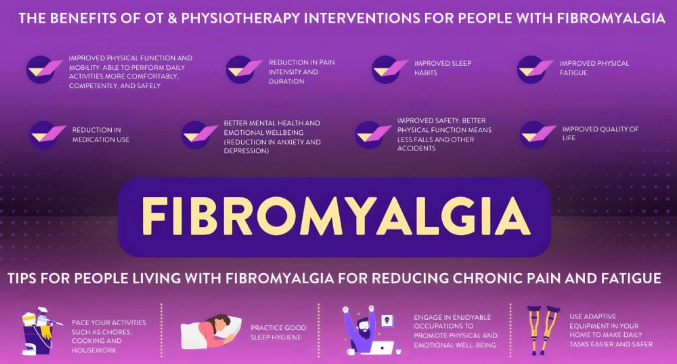
How Society Can Improve Support for Fibromyalgia Patients
To reduce stigma and improve fibromyalgia care, society must:
- Educate the public about fibromyalgia as a legitimate medical condition.
- Train healthcare professionals to recognize and treat fibromyalgia effectively.
- Encourage workplace accommodations for chronic pain conditions.
- Challenge gender bias in pain treatment and diagnosis.
- Increase mental health support for those struggling with the emotional impact of fibromyalgia.
A more inclusive and informed society can significantly improve the lives of fibromyalgia patients.
Conclusion
The impact of society and culture on fibromyalgia extends beyond medical treatment—it affects how patients are perceived, diagnosed, and supported in their daily lives.
While awareness has improved, stigma, misinformation, and healthcare disparities remain significant obstacles. By challenging misconceptions, advocating for better policies, and increasing public education, society can create a more supportive and compassionate environment for people living with fibromyalgia.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores