Introduction
Fibromyalgia is a chronic condition that causes widespread musculoskeletal pain, fatigue, and hypersensitivity to touch. Among the many affected areas, the knees are a common site for tender points, leading to stiffness, aching, and difficulty with movement.
The knee joint plays a crucial role in mobility, making walking, climbing stairs, and even sitting for long periods challenging when fibromyalgia-related knee pain flares up. Many individuals with fibromyalgia mistake knee tenderness for arthritis or joint damage, but this pain is often caused by neurological dysfunction and heightened pain sensitivity, rather than structural issues.
This article explores the causes, symptoms, and best management strategies for knee tender points in fibromyalgia, helping individuals find relief and regain mobility.
What Are Tender Points in Fibromyalgia?
Tender points in fibromyalgia are specific areas on the body that are extremely sensitive to touch and pressure. Unlike general joint pain, these points react sharply to even light pressure, causing localized pain that can radiate to surrounding muscles and ligaments.
The knees are one of the most commonly affected areas, making daily activities painful and difficult for many fibromyalgia patients.
Where Are the Knee Tender Points Located?
Fibromyalgia-related knee tender points are typically found:
- Just above or below the kneecap (patella).
- On the inner side of the knee joint (medial knee region).
- At the outer part of the knee where tendons and muscles attach.
- Along the lower thigh muscles leading into the knee.
These points are symmetrical, meaning they occur on both knees rather than just one side.
Why Are the Knees So Sensitive in Fibromyalgia?
Several factors contribute to knee tenderness in fibromyalgia, including:
- Overactive pain receptors, which increase sensitivity to pressure.
- Muscle tightness and spasms, causing tension around the knee joint.
- Poor blood circulation, leading to stiffness and discomfort.
- Inflammation in the surrounding soft tissues, increasing pain.
Common Symptoms of Knee Tenderness
- Sharp pain when touching or pressing the knee area.
- Aching or burning discomfort in the knee joint.
- Weakness in the legs, making standing or walking difficult.
- Pain that worsens with prolonged sitting or standing.
- Stiffness in the morning or after periods of inactivity.
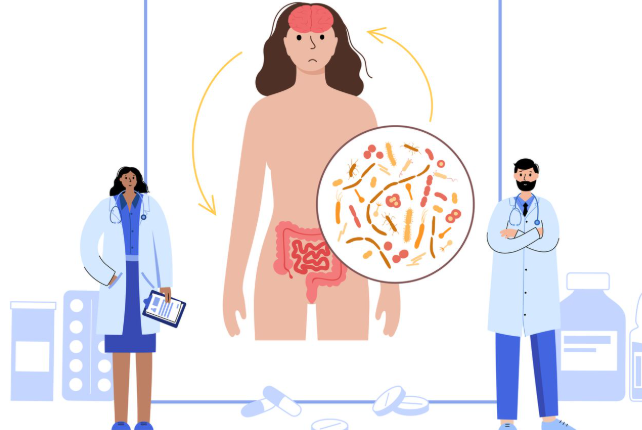
The Role of Central Sensitization in Knee Pain
Fibromyalgia involves central sensitization, where the brain overreacts to pain signals, making the knees more sensitive than normal.
- Mild pressure on the knees can feel intensely painful.
- Pain may persist longer than expected after movement.
- Changes in weather, stress, or fatigue can worsen knee pain.
How Muscle Tension and Nerve Dysfunction Affect the Knees
- Fibromyalgia causes chronic muscle tightness in the legs and thighs, leading to knee pain.
- Nerve hypersensitivity may create a tingling or burning sensation around the knee.
- Inflammation in the surrounding ligaments increases discomfort.
The Connection Between Knee Tender Points and Leg Weakness
- Chronic knee pain can lead to muscle fatigue and leg weakness.
- Tender points restrict movement, making walking difficult.
- Strengthening exercises may help improve function and reduce discomfort.
How Weather Changes Can Worsen Knee Pain
- Cold weather can cause increased stiffness and discomfort in the knees.
- Humidity and barometric pressure changes can intensify knee pain.
- Using warm clothing and heating pads can help manage weather-related flare-ups.
The Impact of Stress and Fatigue on Knee Tenderness
- Stress triggers muscle tension, increasing knee pain.
- Fatigue reduces the body’s ability to recover from pain flare-ups.
- Relaxation techniques can help reduce stress–related pain.
Diagnosing Fibromyalgia-Related Knee Tenderness
Doctors diagnose fibromyalgia-related knee pain by:
- Applying gentle pressure to the knee tender points.
- Assessing widespread pain throughout the body.
- Ruling out conditions like arthritis, bursitis, or tendonitis.
Medications for Managing Knee Tender Points
Common medications for fibromyalgia-related knee pain include:
- Pain relievers (Acetaminophen, NSAIDs).
- Muscle relaxants (Cyclobenzaprine) to ease stiffness.
- Antidepressants (Duloxetine, Amitriptyline) to regulate pain perception.
Physical Therapy and Strengthening Exercises
- Gentle knee stretches to improve flexibility.
- Low-impact exercises like swimming or walking.
- Strengthening exercises for the quadriceps and hamstrings.
Massage Therapy and Myofascial Release for Knee Pain
- Massage therapy can relieve tight muscles and improve circulation.
- Myofascial release can help loosen connective tissues.
- Trigger point therapy may reduce localized pain in the knees.
The Role of Heat and Cold Therapy in Pain Relief
- Applying heat can relax stiff knee muscles.
- Cold therapy can numb sharp pain and reduce inflammation.
Ergonomic Adjustments to Reduce Knee Strain
- Use cushioned shoes to reduce knee pressure.
- Avoid prolonged sitting or standing to prevent stiffness.
- Use supportive knee braces if needed.
FAQs About Knee Tender Points in Fibromyalgia
- Why does fibromyalgia cause knee pain?
- The knees have many pain-sensitive nerves and muscles, making them prone to stiffness and discomfort.
- Can stretching help relieve knee tenderness?
- Yes, gentle stretching improves flexibility and reduces stiffness.
- Can stress worsen knee pain?
- Yes, stress increases muscle tension and pain sensitivity.
Conclusion
Knee tender points in fibromyalgia can be painful and limiting, but with proper management strategies, relief is possible. A combination of medication, physical therapy, stress reduction, and ergonomic adjustments can reduce knee pain and improve daily function.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores