Fibromyalgia is a chronic disorder that predominantly causes widespread pain, fatigue, and cognitive disturbances, which can significantly impact a person’s quality of life. However, individuals living with fibromyalgia may also experience a variety of other symptoms that are not as commonly associated with the condition. One such issue that can occur in fibromyalgia patients is hemorrhoids. While hemorrhoids are a common condition, their occurrence in people with fibromyalgia can complicate the overall symptom management. This article explores the connection between fibromyalgia and hemorrhoids, how hemorrhoids may present in fibromyalgia patients, and how to manage the symptoms effectively.
Understanding Hemorrhoids and Fibromyalgia
Hemorrhoids are swollen veins in the lower rectum or anus, similar to varicose veins, and can be internal or external. The condition can lead to discomfort, pain, bleeding, and itching. Hemorrhoids are a widespread issue, with common causes including chronic v, straining during bowel movements, pregnancy, and obesity. However, there are additional factors that may increase the likelihood of developing hemorrhoids in individuals with fibromyalgia.
Fibromyalgia, on the other hand, is a condition that is not limited to musculoskeletal pain but can also involve gastrointestinal issues, sleep disturbances, and increased sensitivity to stimuli. While fibromyalgia does not directly cause hemorrhoids, it can create conditions that make individuals more susceptible to developing or exacerbating hemorrhoids.
How Fibromyalgia Contributes to Hemorrhoid Symptoms
1. Chronic Constipation
One of the most significant connections between fibromyalgia and hemorrhoids is the gastrointestinal disturbances that often accompany fibromyalgia. Many individuals with fibromyalgia experience chronic constipation, which can put excess pressure on the veins in the lower rectum during bowel movements. This straining increases the likelihood of developing hemorrhoids.
Additionally, the medications frequently prescribed for fibromyalgia—such as opioid painkillers, muscle relaxants, and antidepressants—can contribute to constipation by slowing bowel movements. This creates a cycle where the constipation worsens, leading to more straining and, consequently, an increased risk of hemorrhoids.
2. Sedentary Lifestyle
Fibromyalgia often leads to fatigue, pain, and decreased physical activity, which can contribute to a sedentary lifestyle. Physical inactivity can slow down digestion, reduce blood circulation, and cause the veins in the rectal area to become more vulnerable to swelling. A sedentary lifestyle may thus aggravate the formation of hemorrhoids or worsen existing ones in individuals with fibromyalgia.
3. Increased Stress and Anxiety
Stress is a common symptom of fibromyalgia, and individuals with the condition often experience heightened anxiety and emotional distress. Stress can contribute to gastrointestinal issues, such as irritable bowel syndrome (IBS) and constipation, both of which are risk factors for hemorrhoids. Moreover, stress can also exacerbate fibromyalgia pain, creating a vicious cycle of discomfort and further straining during bowel movements, thus worsening hemorrhoid symptoms.
4. Medications for Pain Relief
Many individuals with fibromyalgia rely on pain relievers to manage their symptoms. Some of these medications, particularly NSAIDs and opioids, can negatively affect digestion and lead to constipation, as previously mentioned. Additionally, these medications can irritate the digestive tract and contribute to a variety of gastrointestinal issues that may increase the risk of hemorrhoids.
Common Hemorrhoid Symptoms in Fibromyalgia Patients
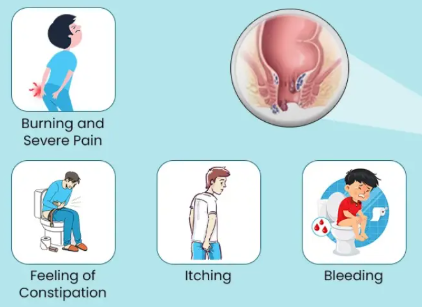
Hemorrhoids present with a variety of symptoms that can be uncomfortable and distressing. When individuals with fibromyalgia develop hemorrhoids, the following symptoms may be experienced:
1. Pain and Discomfort
The hallmark symptom of hemorrhoids is pain, which can range from mild discomfort to sharp, throbbing sensations, especially during or after bowel movements. For individuals with fibromyalgia, who are already dealing with chronic pain, the addition of hemorrhoid pain can amplify the discomfort, making it difficult to distinguish between the pain caused by fibromyalgia and that caused by hemorrhoids.
2. Rectal Bleeding
Bleeding is another common symptom of hemorrhoids, typically occurring when passing stools. The blood may be bright red and seen on toilet paper or in the toilet bowl. In fibromyalgia patients, who may already experience gastrointestinal distress, rectal bleeding can raise concerns and complicate the management of both conditions.
3. Itching and Irritation
Itching around the anus or in the rectal area is a common symptom of hemorrhoids. This sensation can be intensified in fibromyalgia patients due to heightened sensitivity to pain and discomfort. Itching can also lead to scratching, which may worsen the irritation and increase the risk of infection.
4. Swelling or Lump Around the Anus
Swollen veins in the anal area can form into lumps or protrusions, which may be uncomfortable or painful to the touch. These lumps may be internal or external, and in severe cases, they can cause difficulty sitting or moving around. For fibromyalgia patients who already struggle with mobility due to widespread pain, hemorrhoid-related swelling can further limit their ability to carry out daily activities.
5. Changes in Bowel Movements
Hemorrhoids can alter bowel habits, leading to either diarrhea or constipation. Individuals with fibromyalgia who are already dealing with irritable bowel syndrome (IBS) or slow bowel motility may find that hemorrhoids exacerbate these conditions, leading to more frequent or painful bowel movements. This creates an ongoing cycle of constipation, straining, and hemorrhoid flare-ups.
Diagnosing Hemorrhoids in Fibromyalgia Patients
Diagnosing hemorrhoids in individuals with fibromyalgia requires a thorough medical history and physical examination. Because fibromyalgia symptoms can overlap with gastrointestinal symptoms, it is essential for healthcare providers to differentiate between symptoms of fibromyalgia, hemorrhoids, and other potential causes of discomfort.
In many cases, a visual examination may be sufficient to identify external hemorrhoids, while internal hemorrhoids may require further evaluation through a digital rectal exam or anoscopy. If rectal bleeding is present, additional tests may be performed to rule out other gastrointestinal issues, such as colorectal cancer or inflammatory bowel disease.
Managing Hemorrhoids in Fibromyalgia Patients
Managing hemorrhoids in the context of fibromyalgia requires a multi-faceted approach, focusing on both symptom relief and underlying factors such as constipation, stress, and medication use.
1. Dietary Changes
A high-fiber diet is essential for maintaining healthy digestion and preventing constipation, a major contributor to hemorrhoids. Fruits, vegetables, whole grains, and legumes should be incorporated into the daily diet to soften stools and promote regular bowel movements. Staying hydrated is also crucial, as water helps prevent dehydration, which can lead to constipation.
2. Regular Physical Activity
For individuals with fibromyalgia, low-impact exercises such as walking, swimming, or yoga can improve digestion and circulation. Exercise can also reduce stress and fatigue, which may help alleviate both fibromyalgia and hemorrhoid symptoms.
3. Pain Management for Hemorrhoids
Topical treatments such as hemorrhoid creams or suppositories containing hydrocortisone can reduce inflammation and soothe itching and discomfort. For more severe cases, healthcare providers may recommend procedures like rubber band ligation, sclerotherapy, or hemorrhoidectomy to remove or shrink hemorrhoids.
4. Medications for Constipation
In fibromyalgia patients, medications that address constipation—such as laxatives or stool softeners—can help ease the passage of stools, reducing straining during bowel movements. It is important to consult a healthcare provider before using these medications, especially if they may interact with fibromyalgia medications.
5. Stress Management Techniques
Since stress exacerbates both fibromyalgia and gastrointestinal issues, engaging in stress-reduction practices like meditation, deep breathing exercises, and cognitive-behavioral therapy (CBT) can provide relief. Reducing overall stress can help manage both conditions simultaneously.
Conclusion
Hemorrhoids are a common and uncomfortable condition that can be more complicated to manage in individuals with fibromyalgia. The overlapping symptoms of gastrointestinal distress, chronic constipation, and pain sensitivity can make it difficult for individuals to distinguish between the two conditions. However, with proper dietary management, physical activity, pain relief options, and stress-reduction techniques, it is possible to manage both fibromyalgia and hemorrhoids effectively, improving overall well-being and quality of life.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores