Introduction
Fibromyalgia is a complex chronic disorder primarily known for causing widespread pain, fatigue, and cognitive difficulties. However, many people with fibromyalgia also experience unexplained sensory issues, including hearing loss, tinnitus, and sound sensitivity.
Although fibromyalgia itself is not a direct cause of hearing loss, research suggests that the condition’s impact on the nervous system, circulation, and inflammation could contribute to auditory dysfunction. Additionally, certain medications used to manage fibromyalgia symptoms may have ototoxic effects, meaning they can damage hearing over time.
This article explores the connection between fibromyalgia and hearing loss, discusses key symptoms, and provides management strategies to help maintain ear health.
1. Understanding Hearing Loss in Fibromyalgia
Hearing loss refers to a partial or complete inability to hear sounds in one or both ears. It can occur gradually or suddenly, depending on the underlying cause.
People with fibromyalgia often report changes in their hearing, including difficulty understanding speech, sensitivity to certain sounds, and episodes of muffled hearing. These symptoms may stem from neurological dysfunction, chronic inflammation, circulatory issues, or medication side effects.
1.1 Types of Hearing Loss
Hearing loss in fibromyalgia can present in different ways:
- Sensorineural Hearing Loss (SNHL): Occurs when the inner ear or auditory nerve is damaged, leading to permanent hearing impairment.
- Conductive Hearing Loss: Results from a blockage or dysfunction in the outer or middle ear, such as ear infections, fluid buildup, or inflammation.
- Mixed Hearing Loss: A combination of both sensorineural and conductive hearing issues.
Some fibromyalgia patients may experience temporary hearing difficulties, while others notice progressive decline in their auditory function.
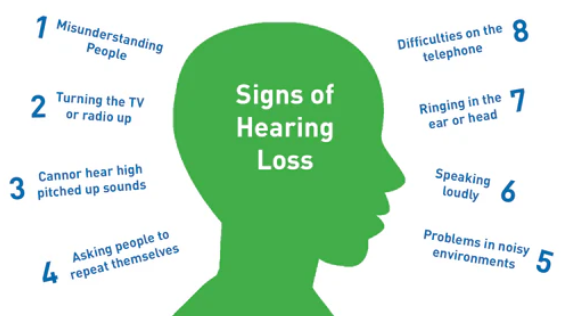
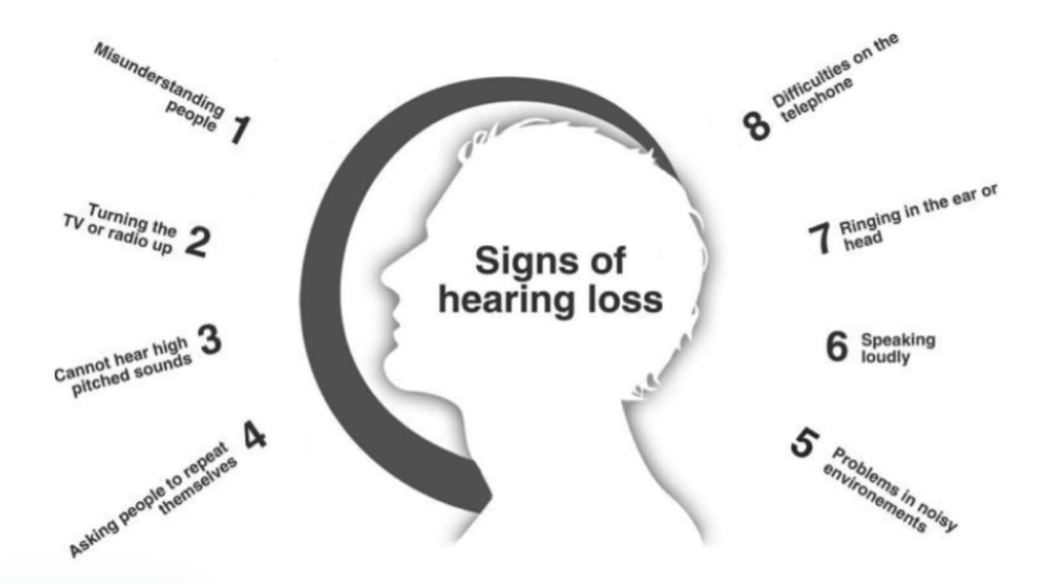
2. Common Hearing Loss Symptoms in Fibromyalgia
Many people with fibromyalgia do not immediately associate their hearing problems with their condition. Below are some of the most commonly reported symptoms:
2.1 Difficulty Hearing Conversations
- Struggling to understand speech, especially in noisy environments.
- Frequently asking people to repeat themselves.
- Feeling that voices sound muffled or distant.
2.2 Sensitivity to Sound (Hyperacusis)
- Increased discomfort or pain in response to loud sounds.
- Feeling overwhelmed in crowded or noisy places.
- Certain frequencies or pitches becoming unbearably loud.
2.3 Tinnitus (Ringing in the Ears)
- Hearing a ringing, buzzing, hissing, or clicking sound with no external source.
- Tinnitus may worsen during fibromyalgia flares or high-stress periods.
2.4 Ear Pressure and Fullness
- A sensation of fullness or congestion in the ears without an actual blockage.
- Fluctuating hearing ability, where sounds become muffled and then return.
2.5 Dizziness and Balance Problems
- Some people with fibromyalgia experience inner ear dysfunction, leading to vertigo, dizziness, and unsteadiness.
- Ear infections or inflammation may contribute to balance issues.
2.6 Sound Distortion
- Voices and sounds may seem distorted, robotic, or unnatural.
- Difficulty distinguishing between different sounds, making it hard to focus on conversations.
Hearing problems in fibromyalgia can be temporary or persistent, depending on the underlying causes. Identifying triggers and managing symptoms can help prevent worsening auditory dysfunction.
3. Why Fibromyalgia Patients Experience Hearing Loss
While fibromyalgia does not directly cause hearing loss, several factors can contribute to auditory dysfunction:
3.1 Nervous System Dysfunction
- Fibromyalgia affects the central nervous system, which may disrupt the auditory pathways responsible for processing sound.
- Increased nerve sensitivity and misfiring signals may lead to sound distortion, tinnitus, and temporary hearing difficulties.
3.2 Poor Circulation
- Fibromyalgia is associated with circulatory issues, including reduced blood flow to the ears.
- Inadequate blood supply can damage cochlear hair cells, leading to hearing impairment over time.
3.3 Chronic Inflammation
- Systemic inflammation may affect the inner ear, leading to fluid buildup, pressure changes, and hearing difficulties.
- Some fibromyalgia patients develop coexisting autoimmune conditions, such as Sjogren’s syndrome, which can cause ear and sinus problems.
3.4 Medication Side Effects
- Certain fibromyalgia medications, such as antidepressants, NSAIDs, and muscle relaxants, may have ototoxic effects, leading to tinnitus or hearing loss.
- Long-term medication use can increase the risk of permanent auditory damage.
3.5 Frequent Ear Infections
- People with fibromyalgia may have weakened immune function, making them more prone to ear infections.
- Chronic ear infections can lead to temporary or permanent hearing loss if left untreated.
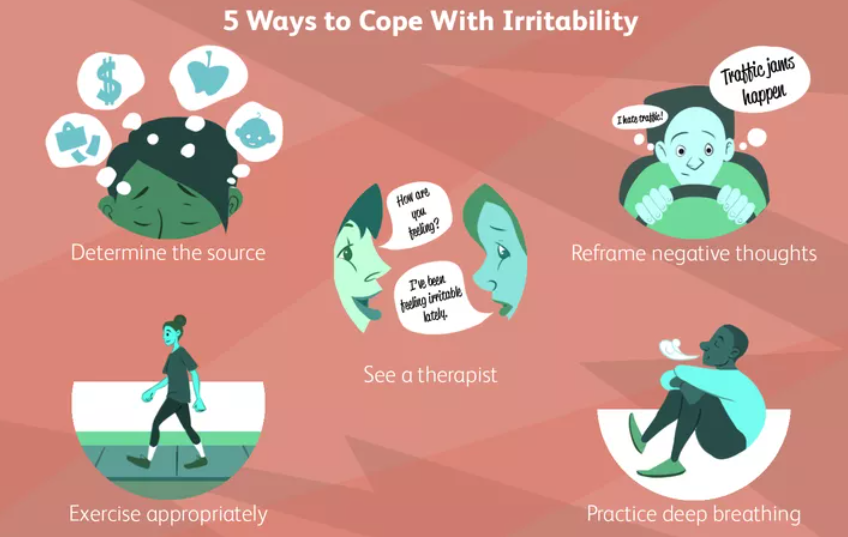
3.6 Stress and Fibromyalgia Flares
- Stress and anxiety can exacerbate hearing symptoms, particularly tinnitus and sound sensitivity.
- Many patients report worsened hearing issues during fibromyalgia flare-ups.
4. How Hearing Loss Affects Fibromyalgia Symptoms
Untreated hearing problems can significantly impact daily life and worsen fibromyalgia symptoms:
4.1 Increased Fatigue and Brain Fog
- Struggling to hear and process conversations requires more mental effort, leading to cognitive exhaustion.
- Hearing loss can contribute to brain fog, memory issues, and difficulty focusing.
4.2 Emotional Distress and Social Isolation
- Miscommunication and difficulty hearing others can lead to frustration, anxiety, and withdrawal from social situations.
- Many fibromyalgia patients already experience depression and anxiety, which may worsen with hearing loss.
4.3 Worsened Sleep Quality
- Tinnitus or heightened sound sensitivity can interfere with sleep, leading to increased pain, fatigue, and irritability.
4.4 Balance and Coordination Problems
- If the inner ear is affected, it may cause dizziness and coordination issues, increasing the risk of falls or injuries.
5. Managing and Preventing Hearing Loss in Fibromyalgia
While fibromyalgia-related hearing issues may not be completely preventable, several strategies can help protect and improve hearing:
5.1 Get Regular Hearing Checkups
- Visit an audiologist or ENT specialist for a hearing assessment if you notice symptoms.
- Early detection can prevent further hearing deterioration.
5.2 Manage Fibromyalgia Symptoms
- Reduce inflammation and nerve sensitivity with an anti-inflammatory diet, gentle exercise, and stress management techniques.
- Stay hydrated and improve circulation with movement and massage therapy.
5.3 Limit Exposure to Loud Noises
- Avoid prolonged exposure to loud environments to protect hearing.
- Use noise-canceling headphones or earplugs when necessary.
5.4 Address Medication Side Effects
- If you suspect medication is affecting your hearing, consult your doctor about alternative options.
5.5 Improve Ear Health
- Avoid ear infections by keeping ears clean and dry.
- Manage sinus issues and allergies that may contribute to ear pressure.
Conclusion
Hearing loss and auditory dysfunction are underrecognized symptoms in fibromyalgia, affecting daily life and overall well-being. While fibromyalgia does not directly cause hearing loss, factors like nervous system dysfunction, poor circulation, chronic inflammation, and medication side effects may contribute to auditory issues.
Recognizing early signs of hearing loss, such as difficulty understanding speech, tinnitus, and ear pressure, can help in preventing further complications. By managing fibromyalgia symptoms, protecting ear health, and seeking professional hearing care, individuals can maintain their quality of life and overall well-being.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores