Introduction: Can the Carnivore Diet Offer Relief from Chronic Pain?
Chronic pain conditions like arthritis and fibromyalgia are notoriously difficult to treat. Many patients cycle through medications, physical therapy, and lifestyle changes, only to experience minimal relief. However, a growing number of people are turning to a radical dietary shift— the carnivore diet—to eliminate inflammation and pain.
The carnivore diet is an all-meat, zero-carb approach that eliminates potential inflammatory triggers found in plant-based foods. Some individuals report significant reductions in joint pain, muscle soreness, and fatigue after switching to this diet. But does science support these claims? This article explores how the carnivore diet may help reduce chronic pain, arthritis, and fibromyalgia symptoms, along with key considerations before making the switch.
Understanding Chronic Pain, Arthritis, and Fibromyalgia
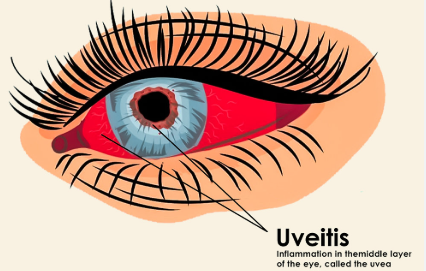
1. The Role of Inflammation in Chronic Pain
Most chronic pain conditions share a common factor—inflammation. Whether caused by an overactive immune system, poor diet, or gut dysfunction, chronic inflammation contributes to:
- Ongoing muscle and joint pain
- Fatigue and cognitive dysfunction (brain fog)
- Increased pain sensitivity (central sensitization)
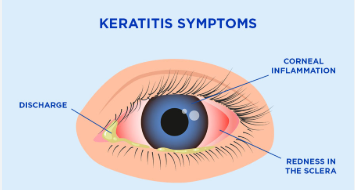
2. Arthritis: When Joint Inflammation Becomes Debilitating
Arthritis refers to joint inflammation and degeneration, leading to pain, stiffness, and reduced mobility. Common forms include:
- Osteoarthritis (OA): Wear-and-tear damage to joints over time
- Rheumatoid arthritis (RA): An autoimmune condition where the immune system attacks joint tissues
3. Fibromyalgia: A Complex Neurological Pain Condition
Fibromyalgia is not caused by joint damage but is linked to nervous system dysfunction, inflammation, and metabolic imbalances. Symptoms include:
- Widespread muscle pain and stiffness
- Chronic fatigue and poor sleep quality
- Hypersensitivity to touch, noise, and temperature
Because diet plays a crucial role in inflammation and nerve health, many people explore nutritional strategies to manage their pain conditions.
How the Carnivore Diet May Help Reduce Chronic Pain
1. Eliminating Inflammatory Plant Compounds
Many plant foods contain natural chemicals that can trigger inflammation, especially in those with autoimmune or pain conditions. These include:
- Oxalates (found in spinach, nuts, and sweet potatoes), which can contribute to joint pain
- Lectins (in beans, legumes, and grains), which can irritate the gut and immune system
- Gluten and plant-based proteins that may contribute to autoimmune flares
By removing all plant-based foods, the carnivore diet eliminates these potential irritants, allowing the body to focus on healing.
2. Reducing Blood Sugar Spikes and Insulin Resistance
Many chronic pain conditions are linked to insulin resistance and unstable blood sugar levels. High blood sugar promotes:
- Increased inflammation throughout the body
- Joint damage and worsening arthritis symptoms
- Energy crashes and heightened fibromyalgia fatigue
The zero-carb nature of the carnivore diet stabilizes blood sugar and lowers insulin levels, which may reduce inflammatory responses linked to chronic pain.
3. Supporting Joint and Muscle Repair with Collagen and Nutrients
Meat-based diets provide essential nutrients that support joint, nerve, and muscle health, including:
- Collagen and gelatin from animal bones and connective tissue, which improve joint flexibility
- Omega-3 fatty acids from fatty meats and fish, which combat inflammation
- Creatine and carnosine, which support muscle function and reduce fatigue
These nutrients are often lacking in plant-based or processed diets, making the carnivore diet an effective way to replenish them.
4. Resetting the Gut Microbiome for Better Inflammation Control
An unhealthy gut microbiome can trigger autoimmune flares, joint pain, and fibromyalgia symptoms. Many people with leaky gut syndrome or food sensitivities report improvements when switching to a carnivore diet because:
- Meat is highly bioavailable and easy to digest
- It eliminates common gut irritants like fiber, gluten, and lectins
- It reduces bloating and digestive discomfort, leading to lower systemic inflammation
Scientific and Anecdotal Evidence Supporting the Carnivore Diet for Pain Relief
1. Case Studies of Arthritis Improvement on a Carnivore Diet
Some arthritis patients have reported:
- Less joint swelling and pain after removing plant foods
- Better mobility and flexibility
- Reduced dependency on pain medications
Research suggests that eliminating inflammatory foods and increasing collagen intake can support joint regeneration and reduce stiffness.
2. Fibromyalgia Patients Seeing Reduced Muscle Pain
People with fibromyalgia following a carnivore diet often describe:
- Fewer pain flare-ups and morning stiffness
- Improved sleep quality
- More stable energy levels
The reduction in gut inflammation and nervous system overstimulation may help explain these benefits.
3. Anti-Inflammatory Effects of a Ketogenic and Zero-Carb Diet
Studies on ketogenic and low-carb diets show that reducing carbohydrate intake can:
- Lower inflammatory markers like C-reactive protein (CRP)
- Improve mitochondrial function, leading to higher energy levels
- Reduce nerve pain by stabilizing blood sugar and insulin levels
Since the carnivore diet is an extreme form of a ketogenic diet, many of these anti-inflammatory benefits are amplified.
How to Start the Carnivore Diet for Pain Management
1. What to Eat
A strict carnivore diet includes:
- Red meat (beef, lamb, pork, bison, venison)
- Fatty fish (salmon, sardines, mackerel)
- Organ meats (liver, heart, kidneys for nutrient density)
- Eggs and high-fat dairy (if tolerated)
- Bone broth and gelatin for joint support
2. What to Avoid
To maximize anti-inflammatory benefits, avoid:
- Processed meats with additives
- Seed oils and vegetable oils
- Sugars and artificial sweeteners
3. Common Side Effects and How to Manage Them
Transitioning to a carnivore diet can cause:
- “Keto flu” (fatigue, headaches) due to carbohydrate withdrawal – Stay hydrated and increase electrolytes
- Digestive changes – Allow time for gut adaptation
- Increased urination and thirst – Drink plenty of water and balance sodium intake
Who Should Be Cautious About the Carnivore Diet?
While many chronic pain sufferers benefit from the carnivore diet, it may not be suitable for everyone. People with:
- Severe kidney disease should consult a doctor due to high protein intake
- Metabolic disorders should monitor blood sugar levels closely
- Autoimmune conditions should transition gradually to prevent flare-ups
Frequently Asked Questions About the Carnivore Diet for Pain Relief
1. How long does it take to see pain relief on the carnivore diet?
Many people report reduced pain and inflammation within a few weeks, but full benefits may take three to six months.
2. Can the carnivore diet reverse arthritis?
While it may not reverse joint damage, it can reduce inflammation, stiffness, and pain, making movement easier.
3. Is the carnivore diet safe for long-term use?
For many people, the carnivore diet is safe when done correctly, but regular bloodwork is recommended to monitor nutrient levels.
4. Will I lose weight on the carnivore diet?
Yes, many people experience weight loss due to reduced inflammation, improved metabolism, and stabilized blood sugar levels.
5. Can I modify the carnivore diet if I am not ready for a full transition?
Yes. Some people start with a ketogenic or low-carb paleo diet before moving toward a strict carnivore approach.
Conclusion: A New Approach to Chronic Pain Management
For those struggling with fibromyalgia, arthritis, and chronic pain, the carnivore diet offers a unique, food-based approach that targets inflammation, blood sugar imbalances, and gut health. While research is still developing, many patients have found relief by eliminating plant-based irritants and focusing on nutrient-dense animal foods.
Anyone considering this diet should consult a healthcare provider, track symptoms carefully, and adjust based on individual responses.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores