Fibromyalgia is a complex, chronic condition characterized by widespread pain, fatigue, and sleep disturbances. While these physical symptoms are commonly known, there are also significant emotional and psychological challenges that come with the condition. One of the lesser-discussed symptoms in fibromyalgia is mood swings. These emotional fluctuations can range from irritability to feelings of sadness and anxiety. In this article, we will explore the connection between fibromyalgia and mood swings, identify the common symptoms, and discuss potential causes and management strategies.
What is Fibromyalgia?
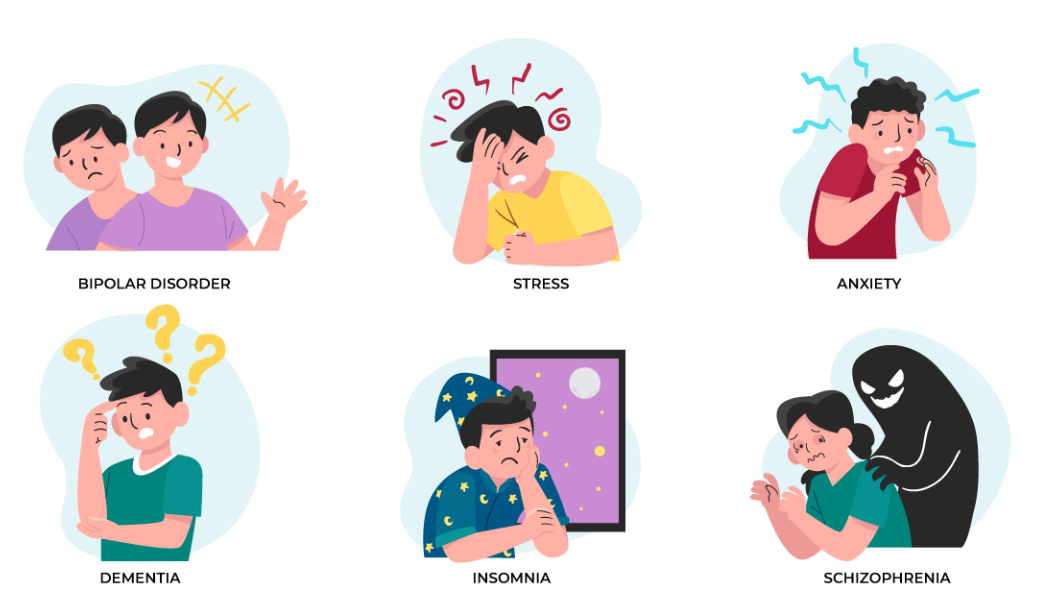
Fibromyalgia is a condition that primarily affects the muscles, tendons, and ligaments, causing widespread pain throughout the body. Other common symptoms include fatigue, sleep disturbances, and cognitive difficulties often referred to as “fibro fog.” While the physical symptoms of fibromyalgia are most well-known, the emotional toll it takes on individuals can be just as significant. People with fibromyalgia often experience a range of emotional symptoms, including mood swings, anxiety, and depression, which can further complicate the management of the condition.
Mood Swings in Fibromyalgia: A Common but Overlooked Symptom
Mood swings in fibromyalgia are a common but often overlooked symptom. These emotional fluctuations can manifest as rapid shifts in feelings, ranging from irritability and frustration to sadness or anxiety. Unlike mood changes that are triggered by external factors, the mood swings in fibromyalgia often seem to occur without a clear cause and can be unpredictable. These emotional shifts can have a significant impact on a person’s ability to manage their condition and their quality of life.
The Connection Between Pain and Mood
One of the primary reasons mood swings occur in fibromyalgia is due to the constant, chronic pain experienced by individuals with the condition. Chronic pain is not only physically exhausting but also mentally and emotionally draining. The ongoing discomfort can lead to feelings of frustration, helplessness, and anger. When these negative emotions are left unaddressed, they can contribute to mood swings.
The Role of Fatigue
Fatigue is another hallmark symptom of fibromyalgia, and it can also contribute to mood swings. People with fibromyalgia often experience overwhelming tiredness, even after a full night’s sleep. This constant fatigue can make it difficult to cope with daily activities and emotional stress. The exhaustion can lead to irritability, low tolerance for frustration, and even feelings of sadness or hopelessness. In some cases, the fatigue can exacerbate feelings of isolation and withdrawal, which can further fuel mood fluctuations.
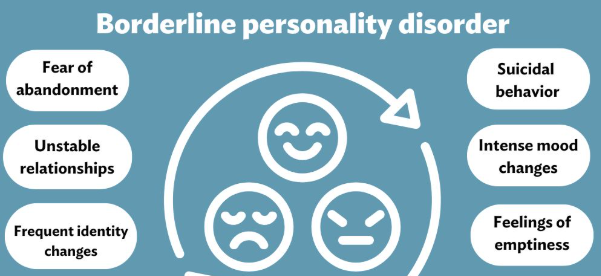
Common Symptoms of Mood Swings in Fibromyalgia
The mood swings associated with fibromyalgia can vary greatly from person to person. While the exact nature of these mood changes differs, common symptoms include:
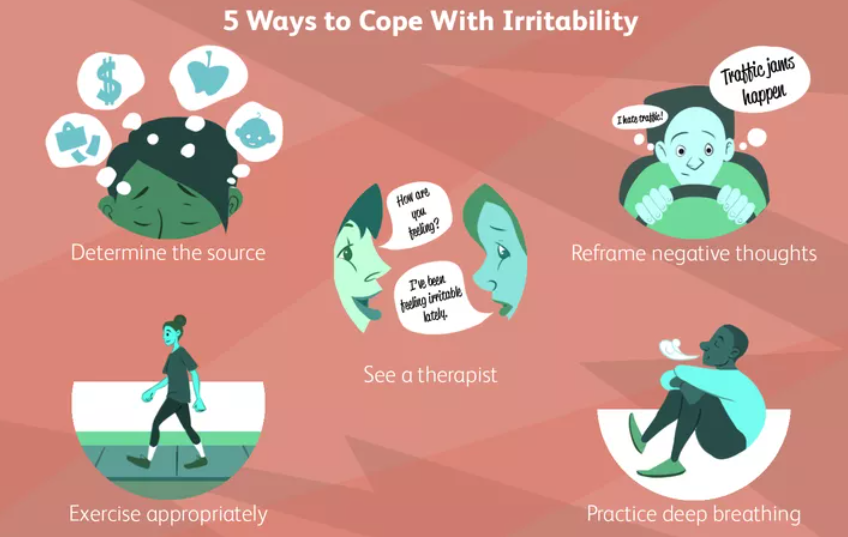
- Irritability and Frustration: Many individuals with fibromyalgia report feeling easily irritated or frustrated, especially when pain or fatigue disrupts their daily activities. This irritability can sometimes lead to conflicts with family, friends, or coworkers, creating additional stress.
- Sadness and Depression: Depression is a common comorbidity in individuals with fibromyalgia. The chronic pain, lack of sleep, and other symptoms can lead to feelings of sadness, hopelessness, or even despair. For some people, these feelings of sadness can escalate into clinical depression, which may require professional treatment.
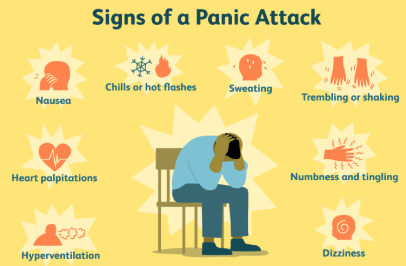
- Anxiety and Worry: Anxiety is another emotional symptom that is frequently reported by individuals with fibromyalgia. The uncertainty of living with a chronic condition can cause significant stress, leading to heightened feelings of anxiety and worry. These feelings may center around concerns about health, daily functioning, or the future.
- Mood Swings Triggered by Sleep Disturbances: Sleep disturbances are a hallmark symptom of fibromyalgia and can greatly influence mood. People with fibromyalgia often experience fragmented or poor-quality sleep, which can leave them feeling irritable, emotionally unstable, or even depressed. The lack of rest exacerbates the emotional challenges, creating a vicious cycle of mood instability.
- Feelings of Isolation: As fibromyalgia symptoms can be invisible to others, many people with the condition experience feelings of isolation. The emotional toll of fibromyalgia can lead to a withdrawal from social situations, which in turn, can lead to loneliness and sadness. These emotions can contribute to the intensity of mood swings.
Potential Causes of Mood Swings in Fibromyalgia
While the exact cause of mood swings in fibromyalgia is not fully understood, several factors are believed to contribute to these emotional fluctuations:
Altered Brain Chemistry
Research suggests that fibromyalgia may be linked to alterations in brain chemistry, particularly in the way the brain processes pain and emotions. The condition may affect the balance of neurotransmitters, such as serotonin and dopamine, which are involved in regulating mood. An imbalance in these chemicals may lead to increased susceptibility to mood swings, depression, and anxiety.
Hormonal Imbalances
Fibromyalgia is more common in women, particularly those of middle age. Hormonal fluctuations, especially those related to menopause, may exacerbate fibromyalgia symptoms, including mood swings. The hormonal changes that occur during this stage of life can affect mood regulation, potentially leading to emotional instability.
Stress and Coping Mechanisms
The chronic pain and fatigue associated with fibromyalgia can cause significant stress, which in turn can contribute to mood swings. Additionally, people with fibromyalgia may have difficulty coping with stress due to limited energy or a lack of support from others. This can lead to emotional dysregulation, making it harder to manage everyday challenges.
Sleep Disruptions
Poor sleep quality is a significant contributor to mood swings in fibromyalgia. Sleep disturbances, which are common in fibromyalgia, can lead to fatigue, irritability, and impaired emotional functioning. Without restorative sleep, the brain and body struggle to regulate emotions, leading to heightened mood instability.
Managing Mood Swings in Fibromyalgia
While mood swings in fibromyalgia are challenging, there are several strategies that individuals can use to manage these emotional fluctuations.
Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a well-established form of therapy that helps individuals recognize and reframe negative thought patterns. CBT can be particularly helpful for managing mood swings, as it teaches people how to cope with negative emotions in a healthier way. Therapy can also address underlying issues such as anxiety and depression, providing tools for emotional regulation.
Medications
In some cases, medications may be prescribed to help manage mood swings. Antidepressants, such as SSRIs (selective serotonin reuptake inhibitors), are commonly used to treat depression and anxiety, which can help stabilize mood. Additionally, medications that address pain and fatigue, such as pain relievers or sleep aids, may also help improve emotional well-being.
Stress Reduction Techniques
Stress management is key to managing mood swings. Techniques such as mindfulness, deep breathing exercises, yoga, and meditation can help reduce stress and improve emotional stability. Regular physical activity, although sometimes challenging due to pain, can also have a positive effect on mood and reduce anxiety.
Improving Sleep Quality
As sleep disturbances are a significant contributor to mood swings, addressing sleep quality is essential. Establishing a consistent sleep routine, practicing relaxation techniques before bed, and creating a sleep-friendly environment can all improve sleep quality and, in turn, help stabilize mood.
Conclusion
Mood swings are a common and often overlooked symptom of fibromyalgia, but they can significantly impact the emotional well-being of those living with the condition. The connection between chronic pain, fatigue, sleep disturbances, and emotional instability makes managing mood swings in fibromyalgia a complex but essential aspect of care. By understanding the underlying causes and employing strategies such as therapy, medication, and stress management, individuals with fibromyalgia can better cope with the emotional challenges and improve their overall quality of life.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores