Fibromyalgia is a chronic pain disorder that affects millions of people worldwide, causing widespread pain, fatigue, sleep disturbances, and cognitive dysfunction. While fibromyalgia is often linked to issues such as low blood pressure, dizziness, and autonomic dysfunction, some patients report experiencing high blood pressure (hypertension).
Although high blood pressure is not a direct symptom of fibromyalgia, research suggests that the nervous system, stress levels, chronic pain, and certain medications may contribute to an increase in blood pressure among fibromyalgia sufferers.
This article explores the potential causes, symptoms, risks, and management strategies for high blood pressure in individuals with fibromyalgia.
1. Can Fibromyalgia Cause High Blood Pressure?
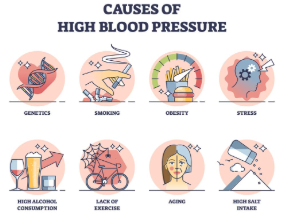
High blood pressure is usually associated with cardiovascular disease, obesity, poor diet, and genetics. However, in fibromyalgia, high blood pressure may be influenced by:
✔ Chronic stress and nervous system dysfunction
✔ Pain-related increases in blood pressure
✔ Medication side effects
✔ Hormonal imbalances and inflammation
While not everyone with fibromyalgia will develop hypertension, those who do may experience greater cardiovascular risks and worsened fibromyalgia symptoms.
2. Possible Causes of High Blood Pressure in Fibromyalgia
Several factors contribute to elevated blood pressure in fibromyalgia patients. These include:
1. Chronic Pain and the Stress Response
✔ Fibromyalgia causes persistent pain, which activates the sympathetic nervous system (fight-or-flight response).
✔ Chronic pain increases cortisol and adrenaline levels, leading to temporary spikes in blood pressure.
✔ Over time, repeated stress responses may contribute to long-term hypertension.
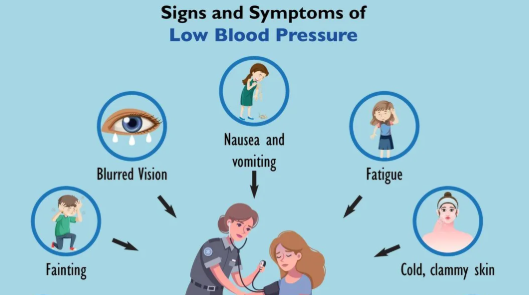
2. Autonomic Nervous System Dysfunction (Dysautonomia)
✔ Fibromyalgia is associated with dysregulation of the autonomic nervous system (ANS), which controls heart rate and blood pressure.
✔ Dysautonomia can cause blood pressure fluctuations, leading to episodes of hypertension or hypotension.
3. Medication Side Effects
✔ Many fibromyalgia treatments, including antidepressants, pain relievers, and corticosteroids, may raise blood pressure.
✔ Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can contribute to fluid retention and increased blood pressure.
✔ Certain antidepressants, like duloxetine (Cymbalta), venlafaxine (Effexor), and amitriptyline, may elevate blood pressure in some individuals.
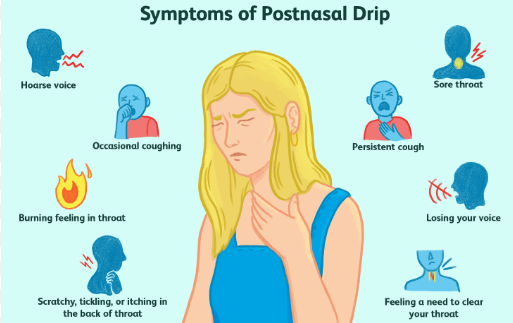
4. Sleep Disturbances and Poor Recovery
✔ Fibromyalgia patients often experience poor sleep quality, insomnia, and sleep apnea.
✔ Disruptions in sleep contribute to increased cortisol levels, which can cause hypertension over time.
5. Inflammation and Hormonal Imbalances
✔ Fibromyalgia is linked to chronic inflammation, oxidative stress, and hormonal imbalances, all of which may impact blood pressure regulation.
✔ Inflammatory markers like C-reactive protein (CRP) are higher in fibromyalgia and have been associated with hypertension risk.
6. Lifestyle Factors
✔ Fibromyalgia patients may experience limited physical activity due to chronic pain and fatigue.
✔ Reduced exercise can weaken cardiovascular function, leading to higher blood pressure over time.
3. Symptoms of High Blood Pressure in Fibromyalgia
Many people with high blood pressure do not experience noticeable symptoms. However, some fibromyalgia patients may report:
✔ Headaches or migraines
✔ Dizziness or lightheadedness
✔ Chest discomfort or palpitations
✔ Shortness of breath
✔ Fatigue or brain fog
✔ Anxiety and heightened stress levels
Because fibromyalgia already causes chronic pain, fatigue, and cognitive difficulties, high blood pressure can worsen these symptoms and further impact daily life.
4. Health Risks of High Blood Pressure in Fibromyalgia
If left unmanaged, hypertension can increase the risk of serious health complications, including:
🚨 Heart disease and heart failure
🚨 Stroke and blood vessel damage
🚨 Kidney disease
🚨 Cognitive decline and memory issues
Since fibromyalgia patients already struggle with chronic pain and fatigue, adding cardiovascular complications can severely impact overall well-being.
5. Managing High Blood Pressure with Fibromyalgia
1. Reduce Stress and Anxiety
✔ Practice relaxation techniques, such as deep breathing, meditation, or progressive muscle relaxation.
✔ Limit caffeine and alcohol, as they can increase stress hormones and raise blood pressure.
✔ Engage in calming activities, like yoga or gentle stretching.
2. Improve Sleep Quality
✔ Follow a consistent sleep routine to support nervous system regulation.
✔ Use magnesium supplements or herbal teas for relaxation.
✔ If you have sleep apnea, seek medical evaluation and consider using a CPAP machine.
3. Monitor Medications
✔ Talk to your doctor about adjusting fibromyalgia medications that may contribute to high blood pressure.
✔ Avoid excessive NSAID use, as they can cause fluid retention and increase BP.
✔ Monitor blood pressure regularly, especially if taking new medications.
4. Maintain a Heart-Healthy Diet
✔ Increase potassium-rich foods (bananas, avocados, spinach) to balance blood pressure.
✔ Reduce processed foods, excess salt, and sugar, which can contribute to hypertension.
✔ Stay hydrated to support cardiovascular function.
5. Engage in Gentle Exercise
✔ Low-impact activities like walking, swimming, and tai chi help regulate blood pressure.
✔ Avoid overexertion, which may trigger fibromyalgia flare-ups.
✔ Start slow and listen to your body.
6. Consider Alternative Therapies
✔ Acupuncture and massage therapy may help relieve pain and reduce stress.
✔ Biofeedback therapy can help monitor and control blood pressure through relaxation techniques.
✔ Supplements like CoQ10, omega-3s, and magnesium may support heart health.
6. Conclusion: Understanding and Managing High Blood Pressure in Fibromyalgia
High blood pressure in fibromyalgia may be linked to stress, pain, nervous system dysfunction, medication side effects, and poor sleep quality.
Although not everyone with fibromyalgia will develop hypertension, those who do should monitor their blood pressure regularly and adopt heart-healthy lifestyle changes.
By focusing on stress management, sleep improvement, dietary adjustments, and gentle exercise, fibromyalgia patients can take proactive steps to maintain a healthy cardiovascular system while managing their chronic pain condition.
Would you like help creating a personalized plan for managing high blood pressure alongside fibromyalgia symptoms?

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores