People with fibromyalgia often ask, “Is fibromyalgia genetic?” It’s a hard question to answer, especially when little is known about how fibromyalgia works. But it’s something that could be relevant to getting the best possible treatment. So let’s look at the evidence.
Is fibromyalgia genetic?
If you have fibromyalgia, there’s a good chance that you know someone in your family who also has it. According to research, fibromyalgia does tend to run in families. And that implies that there is a genetic component to the disease.
The fact that fibromyalgia might be genetic means that the genes that are responsible for so much about the way your body works are passing along fibromyalgia.
But that also means that if someone in your family has fibromyalgia, then you are also likely to develop fibromyalgia.
What does that mean for you?
Because we know that fibromyalgia is genetic, we know that having a relative with fibromyalgia is a red flag when it comes to the possibility of being diagnosed with fibromyalgia. So if someone in your family has the disease, you should keep on guard for the signs that you are also developing it.
Fibromyalgia can’t be cured, but it can be treated. And there’s no reason to spend years suffering without any treatment at all from mysterious aches and pains because you didn’t realize you had the disease.
After all, many people with fibromyalgia can go years before finding out that the cause of their pain is in fact, fibromyalgia.
So with your knowledge of the fact that fibromyalgia is genetic, you can have a better chance of catching it early.
How do I know if I have fibromyalgia?
There are a few warning signs of fibromyalgia that you should watch out for:
If you have any of these symptoms, you should consult a doctor. Tell them if fibromyalgia runs in your family. This will alert them to the possibility that you have fibromyalgia and they should begin tests.
Just remember that the best way to deal with fibromyalgia is to be proactive about managing your symptoms. And get a diagnosis as soon as possible.
Fibromyalgia is a difficult disease to live with. It causes chronic fatigue and pain all over the body. And people who have fibromyalgia often find it hard to find a treatment that works for them. That’s why it’s important to get a diagnosis early so you can get effective treatment as soon as possible. There are a few early signs of fibromyalgia that you should look for to tell if you have fibromyalgia.
Click Here to Visit the Store and find Much More….
What Are The Early Signs Of Fibromyalgia?
Fibromyalgia can be difficult to diagnose. And in the early stages, the first signs of fibromyalgia can be very different for different people. One of the best symptoms to look for early on is chronic fatigue. People with fibromyalgia often feel like they can’t seem to get a good rest no matter how much they sleep. And to make things worse, sleeping can be very difficult by itself.
Just feeling tired all the time is probably worth a trip to your doctor, as chronic fatigue is a symptom of many different conditions.
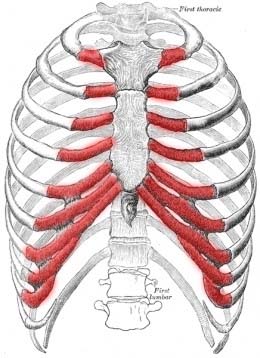
In addition, the most obvious symptom, and the one that doctors use to diagnose you is widespread pain. Fibromyalgia pain is located along 18 different points on the body. These are usually in the joints of the limbs and back. A doctor will test you to see if you have pain in 11 of these points, which is sufficient to prove that you have fibromyalgia.
This pain is typically what causes fibromyalgia patients to visit a doctor, as it is difficult to manage.
What Should You Do If You Think You Have Fibromyalgia?
If you have these early signs of fibromyalgia, it’s important to see a doctor as soon as possible. If possible, it’s best to see a doctor who specializes in fibromyalgia. You can contact the National Fibromyalgia Research Association for a list of fibromyalgia specialists in your area. And a doctor who treats fibromyalgia regularly will be more aware of the early signs of fibromyalgia and better equipped to recommend an effective treatment.
Be honest and thorough when describing your symptoms as it will help the doctor make the best diagnosis possible.
What Are Some Treatments For Fibromyalgia?
There are a number of drugs that doctors prescribe to treat fibromyalgia. Often these are anti-depressants, like Lyrica and Cymbalta, that increase the levels of serotonin in your brain. Serotonin helps calm the nerve pain associated with fibromyalgia.
But there are also other drugs that are new when it comes to treating fibromyalgia but show promise. Drugs like naltrexone offer new hope to people with treatment-resistant fibromyalgia.
And doctors are rapidly testing new drugs and making advancements in the study of what causes fibromyalgia. Meanwhile, many find that the standard treatments are at least partially effective.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores