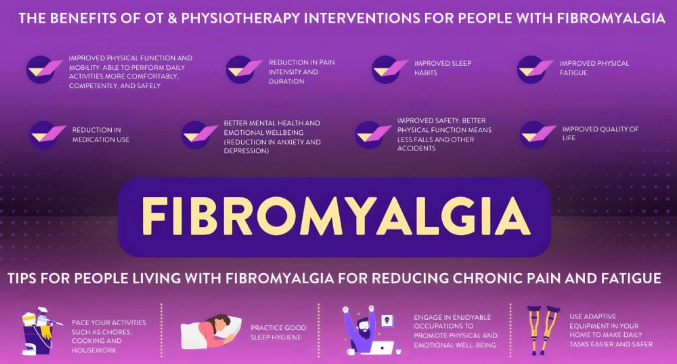
Fibromyalgia is a complex and often debilitating condition characterized by widespread pain, fatigue, sleep disturbances, and cognitive issues. Over the years, various medications have been explored to help manage fibromyalgia symptoms, with gabapentin emerging as a commonly prescribed option. Originally developed to treat epilepsy, gabapentin is now widely used to address nerve-related pain. But how effective is it when it comes to fibromyalgia? In this article, we’ll take a closer look at gabapentin, how it works, and its role in the management of fibromyalgia symptoms.
What Is Gabapentin?
Gabapentin is an anticonvulsant medication that was initially approved for the treatment of epilepsy. It works by calming overactive nerve signals, making it effective for conditions involving nerve pain. Gabapentin is commonly prescribed for neuropathic pain, postherpetic neuralgia (pain after shingles), and restless leg syndrome. Over time, its off-label use for fibromyalgia has grown, as it helps target widespread pain, one of the hallmark symptoms of the condition.
How Gabapentin Works
Gabapentin affects the nervous system by binding to calcium channels in the brain and spinal cord. This action reduces the release of excitatory neurotransmitters, calming overactive nerve activity that contributes to pain. For people with fibromyalgia, this mechanism can help reduce pain signals and potentially improve sleep quality, both of which are often disrupted by the condition.
Gabapentin vs Fibromyalgia: The Evidence
1. Clinical Studies on Gabapentin for Fibromyalgia
Several studies have investigated the effectiveness of gabapentin for managing fibromyalgia symptoms:
- Pain Reduction: Research shows that gabapentin can help reduce widespread pain in fibromyalgia patients. By dampening nerve activity, it decreases the sensation of pain, making it more manageable.
- Improved Sleep: Gabapentin has been linked to improved sleep patterns in fibromyalgia patients, likely due to its calming effect on the nervous system.
- Quality of Life: Some studies indicate that patients taking gabapentin report improvements in overall quality of life, although individual responses vary widely.
2. FDA Approval
While gabapentin is not FDA-approved specifically for fibromyalgia, it is frequently prescribed off-label due to its ability to address some of the condition’s core symptoms, particularly pain and sleep disturbances.
Benefits of Gabapentin for Fibromyalgia
Gabapentin offers several potential benefits for fibromyalgia patients:
- Pain Relief: It can help reduce the intensity of chronic pain, particularly nerve-related pain.
- Better Sleep: By calming the nervous system, gabapentin can improve the ability to fall and stay asleep, which is crucial for managing fibromyalgia.
- Reduced Sensitivity: Many fibromyalgia patients experience heightened pain sensitivity (hyperalgesia). Gabapentin helps moderate this response, making everyday activities more tolerable.
Limitations and Side Effects of Gabapentin
1. Side Effects
Like any medication, gabapentin comes with potential side effects. These include:
- Drowsiness
- Dizziness
- Fatigue
- Weight gain
- Swelling in the hands and feet
- Difficulty concentrating
2. Variable Effectiveness
Gabapentin does not work for everyone. Some patients experience significant relief, while others find little to no improvement in their symptoms. The effectiveness of gabapentin can also depend on the dosage and the individual’s overall health.
3. Tolerance
Over time, some patients may develop a tolerance to gabapentin, meaning higher doses are required to achieve the same level of symptom relief. This can increase the risk of side effects.
Gabapentin vs Other Treatments for Fibromyalgia
Gabapentin is just one of many options for managing fibromyalgia symptoms. Here’s how it compares to other treatments:
1. Gabapentin vs Pregabalin
Pregabalin (Lyrica), a close relative of gabapentin, is FDA-approved for fibromyalgia treatment. While both drugs work similarly, pregabalin has been studied more extensively for fibromyalgia and may have a slight edge in terms of effectiveness. However, gabapentin is often more affordable.
2. Gabapentin vs Antidepressants
Antidepressants like duloxetine (Cymbalta) and amitriptyline are also commonly prescribed for fibromyalgia. These medications target pain, mood, and sleep disturbances, offering a more comprehensive approach. Gabapentin, on the other hand, primarily targets nerve pain and sleep issues.
3. Gabapentin vs Non-Pharmacological Treatments
Non-drug therapies such as exercise, cognitive behavioral therapy (CBT), and acupuncture are often recommended alongside medications like gabapentin. While gabapentin provides symptom relief, these holistic approaches address the root causes and help improve long-term outcomes.
Who Might Benefit from Gabapentin?
Gabapentin may be a good option for fibromyalgia patients who:
- Experience significant nerve-related pain.
- Struggle with sleep disturbances.
- Have not responded well to other treatments like antidepressants or pregabalin.
- Prefer a medication with a sedative effect to improve relaxation and sleep.
Tips for Taking Gabapentin for Fibromyalgia
If you and your healthcare provider decide that gabapentin is the right choice, consider the following tips:
- Start Low, Go Slow: Gabapentin should be started at a low dose and gradually increased to minimize side effects.
- Monitor Side Effects: Keep track of any side effects and discuss them with your doctor.
- Combine with Lifestyle Changes: For the best results, pair gabapentin with other treatments such as gentle exercise, a healthy diet, and stress management techniques.
- Stay Consistent: Take gabapentin as prescribed, and don’t stop suddenly without consulting your doctor, as withdrawal symptoms can occur.
Conclusion: Is Gabapentin the Right Choice for Fibromyalgia?
Gabapentin can be a valuable tool in the management of fibromyalgia symptoms, particularly for those struggling with nerve pain and sleep disturbances. While it is not a cure, it offers relief for many patients, allowing them to regain some control over their daily lives. However, gabapentin is not without its limitations, and it may not work for everyone. As with any fibromyalgia treatment, a personalized, holistic approach that includes lifestyle changes, therapy, and possibly other medications is key to achieving the best possible outcome.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores