Introduction: When Fibromyalgia Affects Only the Left Side
Fibromyalgia is known for causing widespread pain, fatigue, and cognitive difficulties, but some individuals experience symptoms primarily or more intensely on one side of the body—especially the left side.
Although fibromyalgia is generally considered symmetrical, meaning it affects both sides equally, some patients report more severe discomfort, stiffness, or nerve-related symptoms on their left side. This article explores why fibromyalgia might be worse on the left side, the symptoms associated with it, and how to manage this unusual pain pattern effectively.
Can Fibromyalgia Really Affect Just One Side of the Body?
1. The Nature of Fibromyalgia Pain
Fibromyalgia is classified as a neurological pain disorder, meaning that it affects how the brain and spinal cord process pain signals. The condition is typically diagnosed based on widespread pain lasting longer than three months, occurring on both sides of the body and above and below the waist.
However, some patients notice that their symptoms:
- Are significantly worse on one side, particularly the left side
- Start on one side and gradually spread
- Fluctuate in severity, but remain more painful on the left
2. Why Does Fibromyalgia Affect the Left Side More?
There are several possible explanations for why fibromyalgia symptoms may be more intense on the left side of the body:
a) Nervous System Asymmetry
The brain and spinal cord do not always process pain evenly across both sides. Some people naturally experience increased nerve sensitivity on one side due to:
- Differences in nerve signaling between the left and right hemispheres
- Spinal misalignments affecting one side more than the other
- Past injuries or trauma that heightened pain perception on one side
b) Postural and Muscle Imbalances
Many people unconsciously favor one side of their body for daily activities, such as:
- Carrying a bag or backpack on one shoulder
- Sleeping on one side every night
- Using one hand or leg more frequently for movement
These habits can lead to chronic muscle tension, misalignment, and pain patterns that may explain why fibromyalgia symptoms feel worse on the left side.
c) Previous Injuries or Surgeries on the Left Side
If someone has experienced a past injury, surgery, or chronic strain on the left side, the nervous system may develop pain memory patterns, making the area more sensitive to fibromyalgia flare-ups.
d) Trigger Points and Myofascial Pain Syndrome
Many fibromyalgia patients also have myofascial pain syndrome, a condition where tight muscle knots (trigger points) cause localized pain. If these trigger points develop more frequently on the left side, the pain may appear uneven or one-sided.
Symptoms of Left-Sided Fibromyalgia
1. Pain Localized on the Left Side
Those with left-sided fibromyalgia often experience:
- Sharp or aching pain in the left shoulder, arm, or leg
- More intense discomfort in the left side of the neck and jaw
- Hip or lower back pain primarily affecting the left side
2. Numbness and Tingling on the Left Side
Some fibromyalgia patients report numbness, tingling, or a pins-and-needles sensation, especially in:
- The left hand and fingers
- The left foot and toes
- The left side of the face or scalp
3. Stiffness and Limited Mobility
Muscle tightness and joint stiffness may be more severe on the left side, making it difficult to:
- Turn the head fully to one side
- Raise the left arm or rotate the left shoulder
- Walk comfortably without pain in the left leg or hip
4. Sensory Sensitivities on the Left Side
Some fibromyalgia patients experience heightened sensitivity to touch, temperature, or pressure, such as:
- Clothing or bedding feeling irritating on the left side
- Increased pain from cold or hot temperatures affecting the left side
- Discomfort when someone applies light pressure on the left side
How to Manage Left-Sided Fibromyalgia Pain
1. Correcting Muscle Imbalances and Posture
If one-sided muscle tightness or postural habits are contributing to symptoms, simple adjustments may help reduce pain.
Effective strategies include:
- Physical therapy to strengthen weaker muscles and correct imbalances
- Stretching routines targeting the left-sided muscles
- Ergonomic adjustments for workspaces and daily activities
2. Pain Management Techniques for One-Sided Fibromyalgia
Focusing on targeted pain relief for the left side can help improve overall function.
Best treatments include:
- Heat therapy (heating pads or warm baths) to loosen left-sided muscles
- Foam rolling or self-massage to reduce knots and trigger points
- Trigger point therapy to release chronic muscle tension
3. Nerve Pain Management Strategies
If nerve dysfunction is contributing to left-sided symptoms, treatments that support nerve health and function may be beneficial.
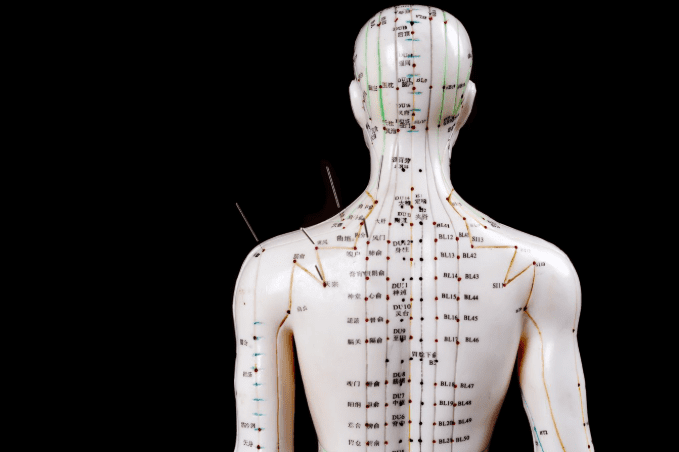
Helpful techniques include:
- Acupuncture or electrotherapy to stimulate nerve repair
- Magnesium supplements to help relax nerves and muscles
- Gentle stretching and nerve gliding exercises to reduce compression
4. Adjusting Sleep Position and Ergonomics
If sleep posture is contributing to left-sided fibromyalgia pain, making small adjustments may help.
Recommendations:
- Using a supportive pillow to keep the spine aligned
- Sleeping on the right side if the left side is more painful
- Placing a pillow between the knees to relieve hip pressure
5. Exploring Central Nervous System Regulation
Since fibromyalgia is linked to nervous system dysfunction, therapies that calm the brain and spinal cord can help reduce pain sensitivity.
Potential approaches:
- Deep breathing exercises to regulate the nervous system
- Low-dose naltrexone (LDN) or nerve pain medications
- Mindfulness and relaxation techniques to lower stress-related muscle tension**
When to Seek Medical Advice
If fibromyalgia pain is significantly worse on the left side, it is important to rule out other medical conditions that may cause asymmetrical pain, such as:
- Nerve entrapment syndromes (sciatica, carpal tunnel, or thoracic outlet syndrome)
- Autoimmune conditions like multiple sclerosis or lupus
- Herniated discs or spinal misalignments affecting one side
A rheumatologist, neurologist, or physical therapist can help determine whether the pain is fibromyalgia-related or due to another issue.
Frequently Asked Questions About Left-Sided Fibromyalgia
1. Can fibromyalgia pain be worse on one side?
Yes. While fibromyalgia typically affects both sides, some patients experience more severe symptoms on one side due to nerve sensitivity, past injuries, or muscle imbalances.
2. Why does my fibromyalgia pain feel worse on my left side?
Possible explanations include:
- Postural imbalances or repetitive strain on the left side
- Nervous system asymmetry causing uneven pain sensitivity
- Previous injuries that created pain memory patterns on the left side
3. How can I relieve left-sided fibromyalgia pain?
Targeted therapies, such as physical therapy, nerve pain management, stretching, and ergonomic adjustments, can help reduce one-sided symptoms.
4. Should I be concerned if fibromyalgia pain is only on one side?
If pain is severe, persistent, or accompanied by new neurological symptoms, seek medical evaluation to rule out nerve damage, autoimmune conditions, or structural issues.
Conclusion: Managing One-Sided Fibromyalgia for Better Relief While fibromyalgia is generally widespread, experiencing left-sided pain more intensely is not uncommon. By identifying the root causes, correcting muscle imbalances, and using targeted pain management strategies, individuals can improve symptom control and overall quality of life. Seeking medical advice for unusual, persistent, or worsening one-sided pain ensures that the right treatment approach is taken.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores