Fibromyalgia is a chronic disorder characterized by widespread pain, fatigue, sleep disturbances, and cognitive dysfunction. Many individuals with fibromyalgia experience a variety of symptoms that can significantly impact their quality of life. One such condition that often complicates fibromyalgia is anemia. Anemia, a condition in which the body lacks enough healthy red blood cells to carry adequate oxygen to tissues and organs, is common among those with fibromyalgia and can worsen many of the symptoms typically associated with the disorder. In this article, we will explore how anemia affects individuals with fibromyalgia, the common symptoms, and strategies for managing both conditions.
Understanding Anemia and Fibromyalgia
Anemia is primarily caused by a deficiency in red blood cells or hemoglobin, which is the protein responsible for oxygen transport in the blood. There are several types of anemia, each with different causes, including iron-deficiency anemia, vitamin B12 deficiency anemia, and anemia due to chronic disease.
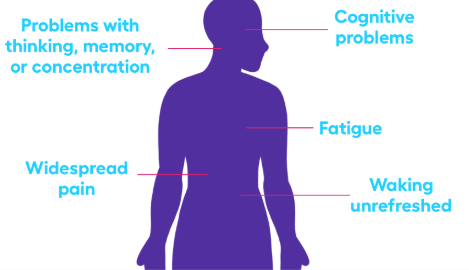
Fibromyalgia, on the other hand, is a complex, chronic condition characterized by musculoskeletal pain, fatigue, and cognitive impairment, often referred to as “fibro fog.” Though the causes of fibromyalgia are not entirely understood, it is believed to involve abnormalities in how the brain processes pain signals, as well as factors such as genetics, trauma, and stress.
Individuals with fibromyalgia are at a higher risk of developing anemia due to various factors, such as nutrient deficiencies, chronic inflammation, and poor absorption of nutrients from food. Moreover, the symptoms of anemia can overlap with those of fibromyalgia, making it challenging to diagnose and manage both conditions effectively.
Common Symptoms of Anemia in Fibromyalgia
The symptoms of anemia can range from mild to severe, depending on the type and severity of the condition. When anemia occurs alongside fibromyalgia, it can amplify existing symptoms and make daily life even more challenging. Below are some common anemia symptoms that are often experienced by individuals with fibromyalgia:
1. Fatigue and Weakness
Fatigue is one of the hallmark symptoms of fibromyalgia, and anemia can exacerbate this symptom. Individuals with both fibromyalgia and anemia often feel unusually tired, even after getting adequate rest. This fatigue can make it difficult to perform normal daily activities, such as working, exercising, or caring for personal needs. The reduced oxygen supply due to anemia can make individuals feel weak and drained, adding to the overall exhaustion that fibromyalgia causes.
How it affects fibromyalgia: Fatigue is already a major challenge in fibromyalgia, and the additional burden of anemia can make the fatigue feel more pronounced, contributing to a vicious cycle of exhaustion.
2. Pale Skin and Pale Mucous Membranes
One of the key signs of anemia is pale skin, especially in the face, hands, and lips. This occurs because anemia reduces the amount of hemoglobin in the blood, causing a decrease in blood flow to the skin. Individuals with fibromyalgia may notice that their skin appears paler than usual, particularly when they feel tired or stressed.
How it affects fibromyalgia: Although pale skin alone may not be a significant fibromyalgia symptom, it may serve as a clue that anemia is present, particularly if there is an increase in fatigue and weakness.
3. Shortness of Breath and Dizziness
Anemia reduces the body’s ability to carry oxygen, leading to feelings of breathlessness or dizziness, particularly during physical activity. Individuals with both fibromyalgia and anemia may notice that they become winded or lightheaded more easily than they did before, even with minimal exertion.
How it affects fibromyalgia: Shortness of breath can be especially debilitating for individuals with fibromyalgia, who already struggle with fatigue and muscle pain. This can further limit their ability to engage in physical activities, making it even more challenging to maintain an active lifestyle.
4. Cold Hands and Feet
Anemia can cause individuals to feel cold, particularly in the extremities. This happens because the reduced number of red blood cells limits blood circulation, especially to the hands and feet. In fibromyalgia, poor circulation is also a common issue, leading to coldness in the limbs.
How it affects fibromyalgia: Cold hands and feet can increase discomfort for those with fibromyalgia, who may already suffer from muscle stiffness, joint pain, and poor circulation. The combination of these symptoms can make it more difficult to stay comfortable.
5. Headaches
Frequent headaches are a common symptom in both fibromyalgia and anemia. The reduced oxygen levels caused by anemia can lead to tension-type headaches or migraines. Individuals with fibromyalgia often experience headaches due to stress, muscle tension, and changes in brain chemistry. When anemia is present, headaches may become more frequent or severe.
How it affects fibromyalgia: The added strain of frequent headaches can worsen the cognitive dysfunction and mood disturbances (e.g., irritability and depression) that many individuals with fibromyalgia already experience.
6. Chest Pain and Heart Palpitations
Anemia can sometimes cause chest pain and an increased heart rate, as the heart has to work harder to deliver oxygen to the body’s tissues. When the heart works harder than usual, it can lead to palpitations, which may be uncomfortable or concerning.
How it affects fibromyalgia: Chest pain and palpitations can contribute to increased anxiety and stress, which are already common in individuals with fibromyalgia. These symptoms may also make it more difficult to distinguish between the pain caused by fibromyalgia and that caused by anemia.
Diagnosing Anemia in Fibromyalgia Patients
Diagnosing anemia in individuals with fibromyalgia can be challenging due to the overlap of symptoms. Fatigue, dizziness, and muscle pain are common to both conditions, and anemia symptoms can often be mistaken for a flare-up of fibromyalgia. It is important to work with a healthcare provider to identify whether anemia is present and determine its underlying cause.
A blood test, including a complete blood count (CBC), is the primary method for diagnosing anemia. This test can measure the number of red blood cells, hemoglobin levels, and other important blood markers. Based on the results, further tests may be conducted to determine the type of anemia (e.g., iron-deficiency anemia, vitamin B12 deficiency, or anemia of chronic disease).
Managing Anemia in Fibromyalgia
Managing anemia alongside fibromyalgia requires a comprehensive approach. Here are several strategies that can help alleviate the symptoms of both conditions:
1. Iron and Vitamin Supplementation
If anemia is caused by an iron deficiency, iron supplements may be recommended by a healthcare provider. In cases of vitamin B12 or folate deficiency, supplementation with these vitamins can help restore optimal levels and improve symptoms. However, it is important to avoid self-diagnosing and taking supplements without medical guidance, as taking excess iron or vitamins can have negative effects.
2. Dietary Changes
A balanced diet rich in iron, vitamin B12, and folate is crucial for managing anemia. Foods like red meat, poultry, fish, leafy green vegetables, fortified cereals, and legumes are excellent sources of these nutrients. Including these foods in the diet can help prevent deficiencies and improve both fibromyalgia and anemia symptoms.
3. Managing Fibromyalgia Symptoms
Effective treatment of fibromyalgia can also help alleviate some of the fatigue and pain that is exacerbated by anemia. Pain management strategies, such as physical therapy, exercise, medication, and relaxation techniques, can help reduce the severity of fibromyalgia symptoms and improve overall well-being.
4. Regular Monitoring and Medical Supervision
It is essential for individuals with fibromyalgia to regularly monitor their health and nutritional status. Routine blood tests and check-ups with a healthcare provider can help identify any nutrient deficiencies early and prevent the worsening of both anemia and fibromyalgia symptoms.
Conclusion
Anemia is a common but often overlooked condition in individuals with fibromyalgia. The overlap of symptoms, such as fatigue, weakness, and cognitive dysfunction, can make it difficult to identify when anemia is present. By understanding the relationship between anemia and fibromyalgia and recognizing the symptoms, individuals can take steps to manage both conditions effectively. With proper diagnosis, nutritional support, and symptom management, individuals with fibromyalgia and anemia can significantly improve their quality of life and regain their energy and vitality.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores