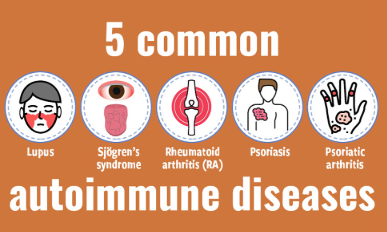
Fibromyalgia is a chronic pain disorder marked by widespread musculoskeletal discomfort, fatigue, cognitive difficulties, and sleep disturbances. Despite growing awareness and improved diagnostic methods, fibromyalgia remains challenging to distinguish from other chronic pain syndromes. Conditions such as chronic fatigue syndrome, rheumatoid arthritis, lupus, myofascial pain syndrome, and neuropathic pain disorders can present overlapping symptoms that often lead to misdiagnosis or delayed treatment.
Accurate differentiation is essential for implementing effective treatment plans, preventing unnecessary testing, and reducing patient frustration. In 2025, clinicians are equipped with refined diagnostic criteria, symptom evaluation tools, and imaging technologies that help clarify the unique characteristics of fibromyalgia. This article outlines how to distinguish fibromyalgia from other chronic pain syndromes and the clinical strategies that lead to precise identification.
Key Features of Fibromyalgia in 2025
Fibromyalgia is now recognized as a centralized pain disorder, meaning it originates from abnormal pain processing in the central nervous system rather than localized inflammation or structural damage. Hallmark symptoms include:
- Widespread musculoskeletal pain on both sides of the body and above and below the waist
- Fatigue that is not relieved by rest
- Cognitive dysfunction known as fibro fog
- Non-restorative sleep
- Mood disorders such as anxiety and depression
- Heightened sensitivity to pressure, noise, and temperature
Diagnosis is based on the Widespread Pain Index (WPI) and Symptom Severity Scale (SSS), without the need for tender point examination. These tools help assess the extent and intensity of symptoms rather than relying solely on physical findings.
Differentiating Fibromyalgia from Similar Conditions
Several chronic conditions mimic fibromyalgia. Here’s how to distinguish fibromyalgia from the most common look-alike disorders.
1. Chronic Fatigue Syndrome (CFS/ME)
Both fibromyalgia and chronic fatigue syndrome present with severe fatigue, cognitive dysfunction, and unrefreshing sleep. However, CFS is typically characterized by post-exertional malaise, where symptoms dramatically worsen after physical or mental exertion. In contrast, fibromyalgia emphasizes pain and sensory sensitivity as the central issues.
- CFS: Primary symptom is fatigue; pain is secondary
- Fibromyalgia: Primary symptom is widespread pain; fatigue is significant but secondary
2. Rheumatoid Arthritis (RA)
RA is an autoimmune inflammatory disorder that causes joint pain, swelling, and stiffness. It can resemble fibromyalgia in its early stages, especially when pain is diffuse. However, RA typically includes elevated inflammatory markers (ESR, CRP) and positive antibodies (RF, anti-CCP), which are absent in fibromyalgia.
- RA: Inflammatory joint damage visible on imaging and labs
- Fibromyalgia: Normal inflammatory markers; pain without joint erosion
3. Systemic Lupus Erythematosus (SLE)
Lupus is another autoimmune disease that affects multiple organ systems. It can cause fatigue, joint pain, cognitive issues, and skin rashes. The presence of photosensitivity, malar rash, and abnormal blood tests (ANA, anti-dsDNA) help differentiate lupus from fibromyalgia.
- SLE: Organ involvement and immune system abnormalities
- Fibromyalgia: No systemic inflammation or organ pathology
4. Myofascial Pain Syndrome (MPS)
MPS involves localized muscle pain due to trigger points in specific muscles. While fibromyalgia affects broader regions, MPS is focused and reproducible. Trigger points in MPS produce referred pain patterns and can be identified through palpation.
- MPS: Regional pain with clear trigger points
- Fibromyalgia: Diffuse pain with no distinct pattern
5. Neuropathic Pain Syndromes
Conditions like small fiber neuropathy or complex regional pain syndrome (CRPS) may be confused with fibromyalgia. Neuropathic pain often involves burning, tingling, and sensory loss, and is confirmed by nerve conduction studies or skin biopsy.
- Neuropathic pain: Follows nerve distribution; sensory deficits present
- Fibromyalgia: Sensory hypersensitivity without neurological deficits
Diagnostic Tools and Clinical Evaluation in 2025
Modern fibromyalgia diagnosis relies on a combination of patient history, validated symptom questionnaires, and exclusion of other conditions. The following tools support clinical decision-making:
- Widespread Pain Index (WPI): Measures pain in 19 body regions
- Symptom Severity Scale (SSS): Evaluates fatigue, sleep, and cognitive symptoms
- Fibromyalgia Impact Questionnaire (FIQ): Measures functional disability and symptom burden
- Blood tests: Rule out inflammation, autoimmune markers, thyroid function, and nutritional deficiencies
- Functional MRI and QST (Quantitative Sensory Testing): Research tools that show central sensitization but are not used routinely
Importance of Patient-Centered Evaluation
Given the subjective nature of symptoms, it is crucial to validate patient experiences while ruling out serious conditions. A thorough evaluation includes:
- Symptom duration and pattern
- Impact on daily life and function
- Psychological and emotional health screening
- Sleep quality and circadian rhythm
- Medication and treatment history
Patients with fibromyalgia often experience stigma and disbelief. Clinicians should approach diagnosis with empathy and openness, explaining that fibromyalgia is a recognized, measurable condition with effective management options.
Treatment Implications of Accurate Diagnosis
Accurate differentiation allows for tailored therapy. Fibromyalgia treatment focuses on:
- Lifestyle interventions: Exercise, sleep hygiene, stress management
- Cognitive behavioral therapy and mind-body practices
- Neuromodulating medications (e.g., SNRIs, pregabalin, low-dose naltrexone)
- Nutritional support and targeted supplements
- Patient education and self-management tools
In contrast, inflammatory or neuropathic conditions require immune-modulating medications, corticosteroids, or nerve-targeted interventions. Misdiagnosis can lead to ineffective treatments and increased symptom burden.
Frequently Asked Questions
1. How long does it take to diagnose fibromyalgia?
It can take months or even years, depending on how symptoms present and whether other conditions are ruled out. New criteria in 2025 help speed up diagnosis with better symptom mapping.
2. Can fibromyalgia occur alongside other chronic pain syndromes?
Yes, it often coexists with conditions like irritable bowel syndrome, migraine, and CFS. This overlap can complicate diagnosis but does not invalidate fibromyalgia.
3. Is there a definitive test for fibromyalgia?
No single test confirms fibromyalgia. Diagnosis is based on clinical criteria, symptom history, and exclusion of other conditions.
4. Are imaging or blood tests useful in diagnosing fibromyalgia?
They are mainly used to rule out other disorders. In fibromyalgia, results are typically normal despite significant symptoms.
5. Why is it important to distinguish fibromyalgia from other conditions?
Each condition requires different treatments. A precise diagnosis ensures patients receive appropriate care and reduces frustration from ineffective therapies.
6. Can fibromyalgia be misdiagnosed as arthritis or lupus?
Yes, especially in early stages. Careful evaluation of symptoms, labs, and disease progression is necessary to avoid misdiagnosis.
Conclusion
Differentiating fibromyalgia from other chronic pain syndromes is a critical step in ensuring proper treatment and improving patient outcomes. In 2025, clinicians have better tools and clearer criteria to recognize fibromyalgia as a distinct central sensitivity disorder. By combining clinical acumen with patient-centered care, accurate diagnosis is not only possible but achievable.
For patients, understanding the differences among conditions helps clarify their journey and empowers them to seek the most effective, personalized treatment strategies. With improved diagnostic clarity, the path to relief and resilience is clearer than ever.
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores