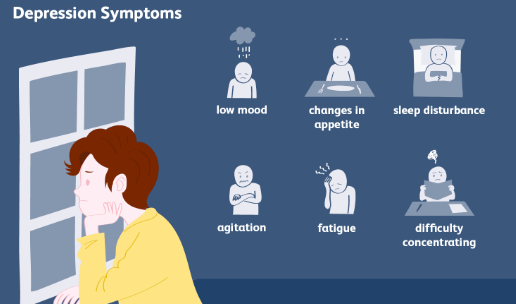
Fibromyalgia is widely recognized as a chronic pain disorder marked by widespread musculoskeletal discomfort, debilitating fatigue, sleep disturbance, and cognitive dysfunction. Traditionally viewed as a non-neuropathic condition due to the absence of clear nerve injury, evolving research suggests that neuropathic pain experienced in fibromyalgia plays a more significant role than previously assumed. This perspective sheds light on the burning, tingling, electric, and stabbing sensations commonly reported by individuals living with fibromyalgia, which mirror symptoms seen in classical neuropathic pain syndromes.
This article explores the characteristics of neuropathic pain in fibromyalgia, its physiological basis, diagnostic implications, and how this evolving understanding can lead to more personalized and effective treatment approaches.
Understanding Neuropathic Pain
Neuropathic pain is defined as pain caused by a lesion or disease of the somatosensory nervous system. It typically presents with symptoms such as:
- Burning or tingling sensations
- Electric shock-like pain
- Numbness or hypoesthesia
- Allodynia, where non-painful stimuli such as touch cause pain
- Hyperalgesia, or increased sensitivity to painful stimuli
This type of pain arises from nerve dysfunction or damage, which alters how sensory signals are transmitted and processed. While fibromyalgia has long been categorized outside of this domain, patient-reported symptoms and emerging evidence challenge this classification.
Overlap Between Neuropathic and Fibromyalgia Pain
Many individuals with fibromyalgia describe sensations that align closely with neuropathic pain descriptors. These may include:
- Numbness or pins-and-needles in the hands, feet, or face
- Burning sensations in specific body regions
- Electric or shooting pains without identifiable cause
- Localized patches of heightened sensitivity or touch intolerance
Though not every person with fibromyalgia experiences these sensations, a significant proportion do, indicating that fibromyalgia may encompass both nociplastic and neuropathic pain components.
Small-Fiber Neuropathy in Fibromyalgia
Recent scientific investigations have discovered that a subset of fibromyalgia patients exhibit evidence of small-fiber polyneuropathy. This condition affects the small unmyelinated nerve fibers responsible for transmitting pain and temperature sensations, as well as autonomic functions.
Evidence of small-fiber involvement in fibromyalgia includes:
- Reduced intraepidermal nerve fiber density in skin biopsies
- Altered quantitative sensory testing results
- Symptoms consistent with burning pain, temperature sensitivity, and paresthesia
Although not universal among all patients, the presence of small-fiber neuropathy in some cases supports the argument that neuropathic mechanisms are present in fibromyalgia and may contribute significantly to its clinical presentation.
Central vs Peripheral Neuropathic Mechanisms
The neuropathic pain experienced in fibromyalgia may arise from both peripheral and central mechanisms.
Peripheral Mechanisms
These involve direct dysfunction or degeneration of peripheral nerves. In fibromyalgia, peripheral sensitization can result from:
- Subclinical inflammation around nerve endings
- Metabolic stress affecting small fibers
- Autoimmune responses directed at peripheral tissues
These factors can sensitize nociceptors, leading to spontaneous pain or exaggerated responses to stimuli.
Central Mechanisms
Central neuropathic pain refers to abnormal processing of pain signals in the spinal cord and brain. In fibromyalgia, the following changes have been documented:
- Hyperactivity in pain-processing regions such as the insular cortex and thalamus
- Altered connectivity in descending pain inhibitory networks
- Imbalance in pain-related neurotransmitters, including serotonin, dopamine, and glutamate
These alterations enhance pain perception even when there is no ongoing peripheral nerve damage, contributing to the chronic and widespread nature of fibromyalgia symptoms.
Diagnostic Challenges
One of the key difficulties in recognizing neuropathic pain in fibromyalgia lies in the limitations of standard diagnostic tools. Neuropathic symptoms in fibromyalgia patients often occur in the absence of observable nerve lesions or abnormalities on traditional imaging and electrophysiological studies.
To identify neuropathic features in fibromyalgia, clinicians may rely on:
- Detailed sensory symptom history using descriptors linked with neuropathic pain
- Screening tools such as the DN4 or PainDETECT questionnaire
- Skin biopsies to evaluate small-fiber nerve density
- Autonomic function testing if dysautonomia is suspected
While these tools are not part of routine fibromyalgia assessment, they can provide crucial information for identifying neuropathic contributions in complex cases.
Treatment Implications of Neuropathic Pain in Fibromyalgia
Recognizing the presence of neuropathic pain components in fibromyalgia has meaningful implications for treatment selection and optimization.
Pharmacologic Interventions
Medications with proven efficacy in neuropathic pain are often beneficial for fibromyalgia symptoms as well. These include:
- Anticonvulsants such as pregabalin and gabapentin, which modulate calcium channels and reduce nerve excitability
- Serotonin-norepinephrine reuptake inhibitors (SNRIs) like duloxetine, which enhance descending pain inhibition
- Tricyclic antidepressants, such as amitriptyline, which can reduce peripheral and central sensitization
- Topical agents, including lidocaine patches or capsaicin cream, for localized neuropathic symptoms
These therapies are more effective than conventional analgesics, as fibromyalgia pain often does not respond well to NSAIDs or opioids.
Non-Pharmacologic Therapies
Addressing neuropathic pain in fibromyalgia also involves non-drug strategies:
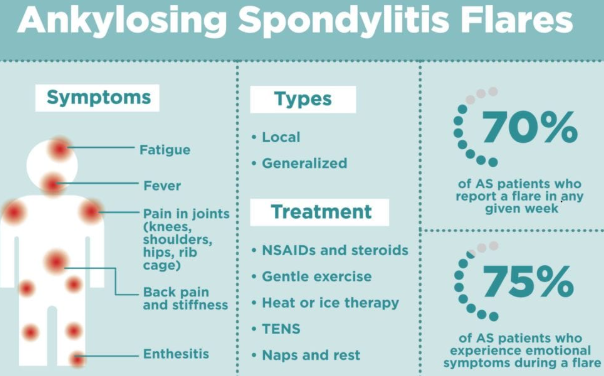
- Transcutaneous electrical nerve stimulation (TENS) to interfere with pain signal transmission
- Mindfulness and meditation, to help reduce central amplification and reactivity
- Graded aerobic exercise, which can improve nerve function and enhance natural pain inhibition
- Cognitive behavioral therapy, targeting maladaptive thoughts and improving pain coping mechanisms
A multidisciplinary approach that includes both pharmacologic and non-pharmacologic modalities offers the best chance for effective symptom management.
Neuropathic Pain as a Validation of Fibromyalgia
The acknowledgment that neuropathic pain experienced in fibromyalgia is not only possible but prevalent challenges earlier misconceptions that dismissed fibromyalgia as purely psychological or medically unexplained. Objective findings such as reduced small-fiber density provide physical evidence of nerve involvement and help validate the lived experiences of patients.
This evolution in understanding not only reduces stigma but also encourages investment in research, diagnostics, and targeted treatment strategies.
Future Research Directions
Ongoing studies continue to investigate the overlap between fibromyalgia and neuropathic pain syndromes. Areas of focus include:
- Identifying genetic variants linked to nerve function and pain sensitivity
- Mapping the interaction between peripheral nerve dysfunction and central sensitization
- Developing biomarkers for early detection of nerve involvement in fibromyalgia
- Testing new therapies that target both neuropathic and nociplastic pain pathways
These research efforts aim to advance a more nuanced and individualized approach to fibromyalgia care.
Conclusion
The neuropathic pain experienced in fibromyalgia represents a critical dimension of this multifactorial disorder. While traditionally excluded from the neuropathic category due to lack of identifiable nerve damage, recent discoveries related to small-fiber involvement and altered central pain processing have redefined the boundaries. Recognizing these neuropathic features allows for more accurate diagnosis, more effective treatment, and a deeper appreciation of the biological complexity of fibromyalgia.
Understanding fibromyalgia as a condition that includes neuropathic pain components fosters a more integrative, respectful, and science-driven approach. It also opens the door to novel interventions that may provide relief for the many individuals navigating life with persistent, unexplained pain. Through continued research and patient-centered care, the goal remains clear: to validate, understand, and improve the quality of life for all those affected by fibromyalgia.
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores