Just imagine that. You’re happy about life. You’re sharing your life with your dream man. You have a couple of kids, a job that most of the time you enjoy, and hobbies and friends to keep you busy. Instead, the mother-in-law is moving in one day.
You don’t know why. You haven’t invited her, and you’re pretty sure, either, that your husband didn’t. You keep thinking she’s going to leave, but you note that her bags have been completely unpacked, and she changes the subject every time you bring up her imminent departure.
Okay, that’s not unlike how I had chronic syndrome of exhaustion. As with most people with CFS, you see, for me, chronic fatigue syndrome came in the form of what I thought was a simple stomach flu. I mentally prepared for a few days of suffering and uncomfortable interruptions, as you would for a short-stay visit with your mother-in-law and believed life would return to normal in a few days. That wasn’t the case. The symptoms took up residence in my body, especially a crushing fatigue, and it would seem five years later that my metaphorical mother-in-law has moved in for good.
It’s not the ideal situation, and it’s one that keeps worrying me, but it’s not all bad news. Some things have been taught to me by the years of living with “her.” I think everybody should know that now that they have this wealth of information.
1st is It’s not all bad to live with CFS.
Like any respectable relationship between MIL and DIL, there are ups and downs in life with chronic fatigue. Sometimes for fear of her wrath, you can’t lift your head off the pillow. But other times, if you walk smoothly, you may go weeks, even months, without a major confrontation.
2nd is It comes with some benefits to live with your Aunt.
The other day I was asked by a friend if I wanted to join her in selling chocolate almonds to the neighborhood. The response was a simple one, “No. Tonight I’m going to entertain my mother-in-law. “Living with this less-than-wanted house guest doesn’t come with many upsides, and now and then I think it’s fair to use it as a (valid) excuse.
Click Here to Visit the Store and find Much More….
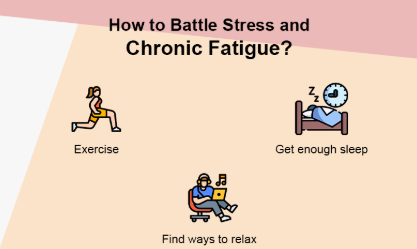
You can’t beat CFS physically or metaphorically, even though you’d like to, as some might “beat” or cure another illness. Some attempts at battling, defying, or otherwise beating it will only make life worse with it. That’s said.
4th is a little kindness is going a long way.
I found it best to show compassion in all respects when coping with this unwelcome resident of my life. A nurturing, peaceful, and patient approach will often yield periods of what is known as “remission” in CFS lingo a period in which symptoms alleviate and one may increase their activity levels.
5th is Do Not involve your Aunt in extreme sports in any circumstances.
CFS ‘ real kicker is a nasty little thing called the post-exertional malaise. Simply put, after taking part in rigorous physical activity, this is the all-kinds-of-terrible you feel 24 to 48 hours. So, while your mother-in-law may seem to enjoy her time on the BMX course, she’ll make you pay later. There’s no going to be any telling what injuries she can get and how long you’ll have to hear about them.
6th is Everything you do: choose your fights.
The condition of chronic fatigue rarely loses a chance to be heard when, say, you’re having a late night with friends or you’re trying to do some hard gardening. Understanding that, when it’s worth it, I’m just going to fight this infection. To me, it means saying no to issues like the community office or the PTA’s voluntary work. But a concert by Garth Brooks? YEAH HELL!
7th is You’re not going to win every fight.
My mother-in-law is a wonderful character. There will certainly be bad times that we call “relapse” in CFS-speaking. I can’t stress enough the ability to accept defeat as the first step towards healing when this happens. I use these moments to drink lots of tea with the MIL for my own sake, reassure her that everything is going to be OK, and convince her to watch Downton Abbey with me until she’s able to bury the hatchet.
8th is Now and then throw her a bone.
It might sometimes feel like your MIL is in need. She needs to relax, today she doesn’t want to dig the weeds, life is too hard for her, she wants to be in bed at 8 p.m. at the earliest. The list continues and continues. Throw her bone now and then, for goodness ‘ sake! Yes. That’s scratching. Give her all her bones, and then some. I promise that you will be worth the pay-off in terms of your safety.
9th is If Aunt comes along, the best of friends won’t mind.
I have always had great friends, but in the last five years I have never appreciated them more. They’re nice and obedient and don’t mind when my mother-in-law wants to slow us down on a vacation — or even if she suggests that we’re staying home instead!
10th is Consider the things that you can’t change.
I didn’t agree with all of this living arrangement. I begged and pleaded with my MIL to reside elsewhere. I even left her stuff on the doorstep, hoping she’d get the hint, but there was no point in it. It seems to stay here, and it’s better to.
11th is You can change some things.
No doubt, it can leave you feeling furious, defeated, and weak when a disease barges into your life unannounced and takes up residence. Nonetheless, for me, there came a point where those emotions had to take a back seat and reflect more constructively on the issues that I could improve. I might be a mother, for example. I would take tai chi, and in reading I could go on a new career. These are activities that I find enjoyable, rewarding, and my “mother-in-law” always finds them quite good!
If one thing with this disease has become apparent during my experience, it is that we are all called to make the best of our living situations. Who knows that? One day I will wake up and may have found other rooms for my metaphorical roommate. But I’m not holding my breath, safe to say. I’m glad to do the best of it for today and take the lessons as they come. How do you cope with the condition of chronic fatigue? Inform me about your observations!

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores