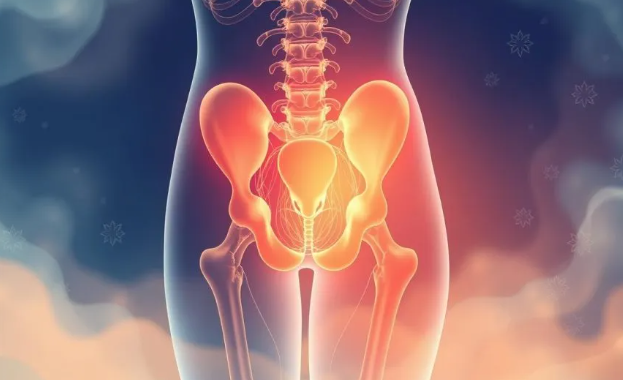
Fibromyalgia is a chronic and often debilitating condition characterized by widespread musculoskeletal pain, persistent fatigue, sleep disturbances, and cognitive dysfunction. For many individuals, conventional treatment options such as antidepressants, anticonvulsants, and pain relievers provide only partial relief and may cause unwanted side effects. This ongoing challenge has led patients and physicians to explore alternative therapies with a better safety profile and fewer adverse effects. Among the most talked-about and researched alternatives is low dose naltrexone for fibromyalgia.
Low dose naltrexone, commonly referred to as LDN, is an off-label use of a medication originally developed to treat opioid and alcohol addiction. However, in smaller doses, it appears to modulate the immune system, reduce inflammation, and enhance pain regulation. This makes it a compelling option for individuals suffering from fibromyalgia who are looking for new solutions.
What is Low Dose Naltrexone
Naltrexone is an opioid receptor antagonist first approved in the 1980s for treating opioid and alcohol dependence. In standard doses of 50 to 100 milligrams, it works by blocking opioid receptors to prevent the euphoric effects of narcotics or alcohol. In low doses, typically between 1.5 and 4.5 milligrams, it works differently.
At these reduced dosages, naltrexone temporarily blocks the body’s opioid receptors, which paradoxically causes a rebound effect. This stimulates the production of endorphins and enkephalins—natural pain-relieving chemicals that also influence the immune system. Over time, this effect may help recalibrate immune function and reduce the chronic pain and inflammation commonly seen in fibromyalgia.
How LDN May Help Fibromyalgia Patients
Several small studies and patient reports suggest that LDN may benefit fibromyalgia patients in a variety of ways. Although research is still ongoing, the following mechanisms are believed to play a role in its effectiveness.
Reduces Central Sensitization
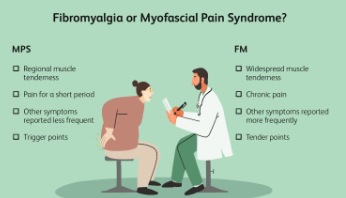
Fibromyalgia is often associated with central sensitization, a condition in which the nervous system becomes hypersensitive and overreacts to pain signals. LDN appears to modulate glial cells in the brain and spinal cord, which are responsible for maintaining inflammation and pain amplification in the central nervous system.
Boosts Endorphin Levels
Low dose naltrexone increases the release of endogenous opioids like endorphins. These chemicals not only reduce pain but also improve mood and energy levels. This can be particularly helpful for fibromyalgia patients who experience both physical and emotional symptoms.
Calms Immune System Dysregulation
LDN may have an immune-modulating effect by reducing pro-inflammatory cytokines and enhancing anti-inflammatory pathways. This is particularly relevant for fibromyalgia, which may involve subtle immune system irregularities contributing to chronic pain and fatigue.
Improves Sleep and Mood
Some patients report improvements in sleep quality, reduction in anxiety, and better emotional resilience when using LDN. These benefits may be linked to increased endorphin activity and decreased inflammatory signals that interfere with restorative sleep.
Dosage and Administration
Low dose naltrexone is typically compounded by a pharmacy, as it is not available in small doses in standard pharmaceutical forms. Most patients begin with a starting dose of 1.5 milligrams taken at bedtime, which is gradually increased to 3 or 4.5 milligrams based on response and tolerance.
Taking LDN at night is thought to be more effective, as this aligns with the body’s natural rhythm of endorphin production. However, timing may vary based on individual response.
It’s essential to use LDN under the guidance of a healthcare provider familiar with its use, especially since it is prescribed off-label and may interact with other medications, particularly opioid-based painkillers.
Potential Benefits Reported by Fibromyalgia Patients
Many people using low dose naltrexone for fibromyalgia have reported the following improvements:
- Reduction in widespread pain
- Better sleep quality
- Decrease in morning stiffness
- Improved mental clarity and reduction in brain fog
- Enhanced mood and reduction in depressive symptoms
- Lowered frequency and intensity of flare-ups
- Improved tolerance for physical activity
Although not everyone experiences the same level of benefit, the low risk of side effects makes LDN a worthwhile option to explore for many.
Side Effects and Considerations
Low dose naltrexone is generally well tolerated. Most reported side effects are mild and often resolve within a few weeks of starting treatment. Common side effects may include:
- Vivid dreams or sleep disturbances
- Headaches
- Mild gastrointestinal upset
- Increased fatigue during the first week
In rare cases, LDN may worsen symptoms before improving them. This paradoxical reaction is typically temporary and may be managed by adjusting the dose or taking breaks.
People currently using opioid medications should not take LDN, as it may block their effectiveness and induce withdrawal. It is important to consult with a physician before beginning LDN therapy.
Availability and Cost
Because LDN is not manufactured in low doses by traditional pharmaceutical companies, it must be compounded by specialized pharmacies. The cost varies depending on the pharmacy and geographic location but is typically much lower than many prescription medications used for fibromyalgia.
Most insurance plans do not cover compounded LDN due to its off-label use. However, the out-of-pocket cost is still relatively affordable, ranging from twenty to forty dollars per month on average.
Research and Evidence Supporting LDN
Several small-scale studies and clinical trials have examined the effects of LDN on fibromyalgia patients. These studies have shown that LDN may significantly reduce pain, fatigue, and inflammation with minimal side effects. Though larger, long-term studies are needed, the early results are promising and have led many physicians to consider it a viable part of a fibromyalgia treatment plan.
Furthermore, ongoing research into LDN for autoimmune and central nervous system conditions continues to build interest and support among both clinicians and patients.
Combining LDN With Other Therapies
LDN can be used alongside other fibromyalgia management strategies, including:
- Physical therapy
- Gentle exercise like yoga or swimming
- Cognitive behavioral therapy
- Nutritional and lifestyle changes
- Supplements such as magnesium or vitamin D
- Non-opioid pain relievers or antidepressants
Its flexibility as a treatment option makes it a strong candidate for integrative fibromyalgia care.
Frequently Asked Questions
1. Is low dose naltrexone approved for fibromyalgia?
No, LDN is not FDA-approved specifically for fibromyalgia, but it is used off-label under physician supervision due to its promising effects on chronic pain and inflammation.
2. How long does it take to see results with LDN?
Some patients notice improvements within a few weeks, while others may take two to three months to see significant changes. Consistency and proper dosing are important.
3. Can I take LDN with other fibromyalgia medications?
LDN can usually be combined with non-opioid medications. However, it should not be used with opioid-based drugs due to potential interactions.
4. What makes LDN different from standard fibromyalgia treatments?
LDN targets inflammation and immune modulation rather than just masking symptoms. It also has a favorable side effect profile compared to many traditional medications.
5. Do I need a special prescription for LDN?
Yes. LDN must be prescribed by a physician and filled by a compounding pharmacy. Standard pharmacies do not carry LDN in the required low doses.
6. Is LDN safe for long-term use?
Current evidence suggests that LDN is safe for long-term use when prescribed appropriately, with no known risk of dependency or tolerance.
Conclusion
Low dose naltrexone for fibromyalgia represents a hopeful shift in chronic pain management. Its unique mechanism of action, combined with a low side effect profile and affordable cost, makes it an attractive option for patients seeking alternatives to traditional drug therapies. While more research is needed to establish standardized protocols and confirm long-term efficacy, early results and patient experiences suggest that LDN has a valuable place in the evolving landscape of fibromyalgia treatment.
For those newly diagnosed or struggling with symptom control, discussing LDN with a knowledgeable healthcare provider could open the door to improved quality of life and renewed optimism.
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores