Fibromyalgia is a complex and chronic pain disorder that affects millions of people worldwide. While its exact cause remains unclear, research suggests that trauma—both physical and emotional—plays a significant role in the development of fibromyalgia. Many individuals diagnosed with fibromyalgia have a history of trauma, including accidents, surgeries, emotional distress, or post-traumatic stress disorder (PTSD).
But how exactly does trauma contribute to fibromyalgia? Does past trauma make someone more susceptible to developing this condition? This article explores the connection between trauma and fibromyalgia, the impact of emotional and physical trauma on chronic pain, and ways to manage trauma-induced fibromyalgia symptoms.
Understanding the Trauma-Fibromyalgia Connection
Trauma, whether physical (injuries, accidents) or emotional (stress, abuse, PTSD), has been linked to chronic pain conditions like fibromyalgia. Many fibromyalgia patients report experiencing a traumatic event before their symptoms began.
Key Theories on How Trauma Leads to Fibromyalgia:
- Central Sensitization: Trauma may cause the brain and nervous system to become hypersensitive, amplifying pain signals and making the body feel pain even when there is no actual injury.
- Dysregulated Stress Response: Trauma can alter the hypothalamic-pituitary-adrenal (HPA) axis, which controls how the body responds to stress, leading to chronic fatigue, pain, and sensitivity.
- Post-Traumatic Stress Disorder (PTSD): Many people with fibromyalgia also have PTSD, suggesting that prolonged emotional distress may trigger neurological changes that contribute to chronic pain.
- Autonomic Nervous System Dysfunction: Trauma can disrupt the autonomic nervous system, causing an overactive fight-or-flight response, which keeps the body in a constant state of tension and pain.
1. Physical Trauma and Fibromyalgia: Can an Injury Trigger Chronic Pain?
Physical trauma, such as car accidents, surgeries, falls, or sports injuries, is often linked to the onset of fibromyalgia symptoms. Many people develop fibromyalgia after a physical injury, even after they have recovered from the initial trauma.
How Physical Trauma Can Trigger Fibromyalgia:
- Nerve Damage: Injuries may cause nerve dysfunction, leading to persistent pain signals.
- Muscle and Tissue Damage: Trauma can cause long-term inflammation, which may contribute to widespread pain.
- Increased Pain Sensitivity: The body may become hypersensitive after trauma, making even minor discomfort feel severe.
Common Symptoms After Physical Trauma:
- Chronic pain that lingers long after an injury heals
- Muscle stiffness and tenderness
- Migraines and tension headaches
- Sleep disturbances and fatigue
How to Cope:
- Seek physical therapy to restore mobility and function.
- Practice pain management techniques, such as massage, acupuncture, and stretching.
- Avoid overexertion to prevent worsening symptoms.
2. Emotional Trauma and Fibromyalgia: The Invisible Connection
Emotional trauma, including childhood abuse, domestic violence, loss of a loved one, or extreme stress, has been strongly linked to fibromyalgia. People with a history of emotional distress are at higher risk of developing chronic pain conditions.
Why Emotional Trauma Contributes to Fibromyalgia:
- Increased Cortisol Levels: Long-term emotional distress can lead to chronic stress and inflammation.
- Nervous System Overload: Emotional trauma may keep the body in a constant state of tension, leading to pain, fatigue, and cognitive dysfunction.
- Sleep Disruptions: Unresolved emotional trauma can cause poor sleep quality, which worsens fibromyalgia symptoms.
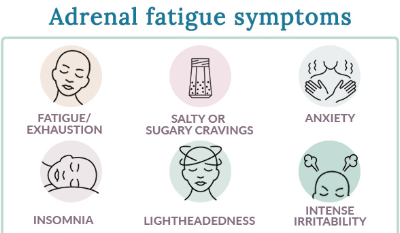
Symptoms of Trauma-Induced Fibromyalgia:
- Heightened pain sensitivity
- Emotional distress (anxiety, depression, PTSD)
- Insomnia and non-restorative sleep
- Memory problems and brain fog
How to Cope:
- Consider therapy or counseling to process past trauma.
- Practice mindfulness techniques, such as meditation and deep breathing.
- Engage in stress-reducing activities, like yoga or journaling.
3. PTSD and Fibromyalgia: A Shared Pathway?
Post-Traumatic Stress Disorder (PTSD) is commonly diagnosed in fibromyalgia patients. Studies suggest that people with PTSD are more likely to develop fibromyalgia, as both conditions involve heightened nervous system responses.
How PTSD and Fibromyalgia Are Linked:
- Overactive Fight-or-Flight Response: PTSD causes chronic hypervigilance, which increases muscle tension and pain.
- Memory and Cognitive Impairment: PTSD and fibromyalgia both contribute to brain fog and difficulty concentrating.
- Emotional Triggers: Stressful events can cause fibromyalgia flare-ups in those with PTSD.
How to Manage PTSD and Fibromyalgia:
- Cognitive Behavioral Therapy (CBT) can help retrain thought patterns.
- Trauma-focused therapy (such as EMDR) may help process past experiences.
- Medication and lifestyle changes can reduce stress-related pain flares.
4. Childhood Trauma and Fibromyalgia: The Long-Term Effects
Childhood trauma, such as abuse, neglect, or severe stress, has been linked to fibromyalgia development in adulthood. People who experience early–life trauma may have altered pain processing systems, making them more prone to chronic pain conditions.
How Childhood Trauma Affects the Body Long-Term:
- Increased Sensitivity to Pain: Childhood trauma may cause lasting changes in pain perception.
- HPA Axis Dysfunction: Early stress disrupts hormone regulation, increasing the risk of chronic pain.
- Mental Health Challenges: Anxiety and depression from childhood trauma can worsen fibromyalgia symptoms.
How to Cope:
- Seek professional therapy to process past trauma.
- Develop a strong support system to manage emotional stress.
- Incorporate relaxation techniques to soothe the nervous system.
Can Trauma Be the Root Cause of Fibromyalgia?
While trauma does not directly cause fibromyalgia, it is considered a major risk factor for developing the condition. Trauma may act as a trigger that leads to nervous system dysfunction, chronic pain, and emotional distress, all of which are hallmarks of fibromyalgia.
Biological Explanations for Trauma-Induced Fibromyalgia:
- Altered Pain Processing: Trauma changes how the brain perceives and responds to pain.
- Increased Inflammation: Chronic stress leads to long-term inflammation and fatigue.
- Impaired Stress Response: Trauma disrupts the nervous system and hormone regulation.
Although trauma can increase the likelihood of fibromyalgia, it is not the sole cause, as genetic, neurological, and environmental factors also play a role.
How to Manage Trauma-Related Fibromyalgia Symptoms
If past trauma is contributing to fibromyalgia symptoms, consider these strategies:
- Therapy and Counseling – Address unresolved emotional trauma.
- Mindfulness and Relaxation – Reduce nervous system overactivity.
- Regular Exercise – Engage in gentle movement to ease tension.
- Healthy Sleep Habits – Improve sleep quality to support healing.
- Medication Management – Consider pain relievers or antidepressants if necessary.
Conclusion: Addressing Trauma to Manage Fibromyalgia
Trauma, whether physical or emotional, can contribute to the onset and severity of fibromyalgia symptoms. While it may not be the sole cause, trauma can sensitize the nervous system, disrupt pain processing, and trigger chronic pain.
By addressing past trauma, managing stress, and adopting a holistic pain management approach, individuals with fibromyalgia can work toward relief and better quality of life.

Click Here to Visit the Store and find Much More….
For More Information Related to Fibromyalgia Visit below sites:
References:
Fibromyalgia Contact Us Directly
Click here to Contact us Directly on Inbox
Official Fibromyalgia Blogs
Click here to Get the latest Chronic illness Updates
Fibromyalgia Stores